The article was published on p. 13-18
Introduction
Epilepsy is rather a common disease which is at the boundary of neurology and psychiatry. The development and application of new antiepileptic drugs let not only improve patient life quality due to seizures control but influence their social functioning as well. However, certain psychiatric disorders, especially in a long-term clinical course, remain an important problem. They can manifest in the form of affective symptoms, behavioral reactions, transitory productive psychopathological disorders, and in some cases — in the form of deficit disorders including dementia.
So far, there is no common well-defined classification of mental disorders in patients with epilepsy. However, aiming to systematize mental abnormalities, most researchers use their attitude to seizures, major clinical presentations, in their works.
Mental disorders are known to occur as a seizure precursor in the frame of aura and as a manifestation of a seizure itself.
Psychic phenomena in the interictal period differ in a variety of disorders. Mood change occurs quite often, less — episodic acute or subacute psychoses. Regarding the development of certain disorders one should take into account individual reactions of a patient to his/her disease as well as society reacting. Currently, borderline psychic disorders occupy a leading place in the clinical picture, they include secondary neurotic ones mainly reflecting peculiarities of an individual response to the disease and being less dependent on epileptic process [2].
The publications dedicated to studying communicative, cognitive, behavioral and social disturbances and their interrelation with permanent local or generalized epileptic activity on the EEG have appeared in recent years [2, 5–8]. Such epileptic activity indicates brain function disorders resulting in changing neuronal combinatorics and information reprocessing. All this results in persistent interictal semiotics manifesting in non-psychotic mental disorders which play a significant role in determining the quality of life of a patient.
This fact, to some extent, moves aside a seizure role and characterological changes (the great importance to which is currently given) resulting in patient’s maladjustment come first.
The development of similar conditions is identical in its mechanism to pathogenesis of epileptic paroxysm realizing through neuron epileptization followed by disintegrating influence on the interactive brain activity, acquiring a prolonged course in 30–80 % of patients [2].
The most common psychopathological comorbid disorder at epilepsy is depression, it is registered in 40–60 % of patients [7, 8]. Depression at epilepsy is a pleomorphic affective disorder manifesting in a variety of symptoms — labile depressive symptoms, depressive behavior, asthenia, sleeplessness, pain, labile affective symptoms (fear, anxiety) and, supposedly, «specific» symptoms (irritability exacerbations, euphoric mood) observed in 70 % of patients [2, 5].
This circumstance dictates the study allowing to connect certain psycho-emotional phenomena to some brain structure lesions or their combinations that causes the impairment of a physiological function performance.
Materials and Methods
We conducted a complex examination of 80 patients suffering from epilepsy. The mean age was 28.9 ± 1.5 years. The inclusion criterion was a reliable diagnosis with an epileptic syndrome and a seizures type defined according to the recommendations of the International League against Epilepsy. All the patients underwent neuroimaging (56 of them — diffuse tensor MRI with tractography) and EEG mapping of the main indices. Multivoxel proton magnetic resonance spectroscopy (1H-MRS) was performed in 28 patients. ICD‑10 criteria were used to identify an interictal depression and an anxiety disorder, and Beck and Spielberg-Khanin tests were used to assess a degree of their severity. The life quality assessment was made with the help of QOLIE‑31 (Quality Of Life In Epilepsy), the assessment of seizures severity was done according to SSQ (Seizure Severity Questionnaire) recommended by the International League against Epilepsy [1].
For statistical manipulations we applied the program package Statistica 6.0 (Wilcoxon criterion, logistic regression, Spearman correlation analysis, Fisher test). The results are presented at the level of confidence significance p < 0.05.
Results
All the patients examined had polymorphic seizures which were combinations of simple, complex partial and generalized paroxysms. The analysis results showed that 55.0 % of the patients complained of emotional lability and only 10.0 % — of dysphoric disorders.
Depression was revealed in 33 of 80 patients (41.3 %) examined according to Beck depression scale. A high level of trait anxiety (TA) was revealed in 36 of 48 (45.0 %) and a high level of situational anxiety — in 29 of 80 (36.3 %) patients examined. According to the results of our investigation, no statistically significant influence of age and education level on developing depression and anxiety disorders was revealed in epileptic patients. There was a significant association of depression with females (r = 0.34, p = 0.045).
The presence of depressive symptoms clearly correlated with the number of seizures per month prior to a therapy (r = 0.42, p = 0.04) as well as with a diagnosed perinatal nervous system lesion detected in past history (r = 0.6, p = 0.005).
The early debut, the disease duration and the history of generalized tonic — clonic seizures proved to be significant factors in the development of anxiety disorders. Other factors showed no significant effect on the occurrence or absence of anxiety and depression symptoms in the patients studied.
In the absence of depression, we found an association with features of an anticonvulsant therapy received during a previous month (a combination of lamotrigine and sodium valproate) (r = 0.54, p = 0.02). Concurrent depression often occurred in patients who earlier had irregularly taken antiepileptic drugs (r = 0.45, p = 0.028). All the patients reported improved mood, attention and social adaptation after changing polytherapy to monotherapy. The reduction of frequency or cessation of seizures as well as the change of their nature to abortive after the beginning of rational therapy significantly correlated with decreasing trait anxiety degree according to Spielberger — Khanin scale.
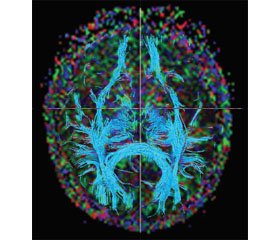
The availability of structural-metabolic disorders is important in the development of depression in patients with epilepsy. First of all, it is the deficit of corpus callosum, fornix and brain stem tracts that is logged when conducting a voxel-morphometry and diffusion tensor imaging [4]. The results got indicate the presence of a larger deafferentation on the side of an epileptic focus (fig. 1).
Depression was significantly associated with the left-sided focus lateralization (r = 0.56, p = 0.022), with the presence of different focal EEG phenomena (spikes (r = 0.53, p = 0.028), of sharp waves (r = 0.52, p = 0.026), of complexes «sharp wave-slow wave» (r = 0.46, p = 0.039), of concomitant trait anxiety (r = 0.48, p = 0.025) and situational anxiety (r = 0.47, p = 0.025).
Clinical remission within a last year appeared to be a precursor of depression lack (OR = 5.86, p = 0.03, χ2 = 4.6).
Precursors of developing depression in epilepsy in the group of adapted patients whom we examined appeared to be the following factors: the EEG phenomenon «sharp wave — slow wave» (OR = 9.6, p = 0.0001, χ2 = 15.11); the presence of epileptic focus EEG lateralization in left hemisphere (OR = 6.67, р = 0.045, χ2 = 3.46); the EEG phenomenon «multiple spikes» (OR = 5.6, p = 0.03, χ2 = 4.46); the female sex (OR = 4.2, p = 0.04, χ2 = 3.95); the high frequency of seizures before a rational therapy (OR = 3.43, p = 0.026, χ2 = 4.9); the availability of seizure focal beginning (OR = 2.1, p = 0.039, χ2 = 4.27).
Thus, despite the rational therapy with anticonvulsants, the absence of seizures or their significant quantity reduction nearly 40.0 % of the epileptic patients socially adapted and not needing hospitalization have anxiety (with trait anxiety prevailing) and depression disorders which require correction.
Our data identified the EEG phenomenon «sharp wave-slow wave» as a major risk factor and the presence of the left-sided epileptic focus laterality as the second most important predictor of depression in patients with temporal lobe epilepsy.
The presence of the EEG phenomenon «multiple spikes» took the third place in importance. It should be emphasized that the highest probability of depression in patients with epilepsy was associated with the availability of disease-specific paroxysmal activity.
According to our results, the female sex is also a predictor of depression in patients with epilepsy.
In our group of surveyed patients we did not reveal the influence of age and education level on the occurrence of depression, although some researchers had noted a statistically significant correlation between low levels of education with the presence of depression due to limitations of social and cognitive activity of an individual [9].
The significance of a high frequency of seizures before a rational therapy and a focal seizure start in developing depression is also consistent with some previous studies. For example, it has been shown that the development of depression is most characteristic of patients with symptomatic focal epilepsy, frequent (more than once a week) seizures, especially with complex partial seizures in temporal lobe epilepsy [7]. A strong correlation between reducing the quality of life for all the items of the questionnaire QOLIE‑31 was identified in patients with depression (r = –0.76) in the presence of high trait (r = –0.82) and high situational (r = –0.7) anxiety (p < 0.0001).
Diffusion tensor MRI with tractography made possible to determine microstructural changes in all our examined patients whereas conventional MRI was informative only in 40.0 % of the cases. In the group of normal volunteers, the most important index of brain white matter integration — fractional anisotropy (FA) — was 0.560 (0.54–0.57) for front quadrants and 0.565 (0.56–0.57) for posterior quadrants. The patients with drug-resistant epilepsy had a bilateral decrease in FA values: for anterior brain parts — 0.52 (0.5–0.55), for posterior ones — 0.53 (0.52–0.54); with the preferential FA reduction being determined in a hemisphere with epifocus (p < 0.05). In patients who were in remission for more than a year, FA value also differed from control ones (p < 0.05), but had no differences compared to the drug-resistant epilepsy group (p > 0.05). At the same time there was a certain relationship between FA in the hemisphere with an epileptic focus and the index of seizure severity according to the questionnaire SSQ (r = –0.38, p < 0.05) that may be a prognostic criterion in assessing the effectiveness of therapeutic interventions.
The correlation analysis revealed a significant relation of the FA values of anterior parts of the hemisphere containing an epileptic focus with the size of central parts of lateral ventricles (r = –0.52, p = 0.009).
In the group of normal volunteers, the values of the mean diffusion capacity index (MDC) were 0.83 (0.80–0.86) for anterior quadrants and 0.85 (0.80–0.88) for posterior quadrants. Compared to the control, MDC in the group of patients in remission was increased in the hemisphere having an epifocus (Z = 2.48, р = 0.013). The obtained results let detect a significant difference in MDC values on the side of an epileptic focus in patients being in sustained remission compared to drug-resistant patients (0.87 (0.84–0.90) and 0.90 (0.86–0.93) for anterior quadrants; 0.88 (0.86–0.89) and 0.90 (0.88–0.91) for posterior quadrants, respectively (р < 0.05)). The given index may be an important factor in prognosing a disease clinical course. We identified a correlation between FA values decreasing (r = –0.46, p < 0.0001) and MDC increasing (r = 0.35, p < 0.0001) homolaterally to an epileptogenic focus and a disease duration.
We identify four distribution clusters of zones with reduced, compared with the control, parameters of fractional anisotropy visualized at tractography: 1) the reduction in representing tracts in anterior brain regions; 2) the mono- or bilateral reduction in representing tracts in external hemisphere parts; 3) the reduction of an anterior and/or a posterior commissure; 4) the combination of the above changes [3].
The presence of these clusters indicates, to some extent, various brain parts «interest» in an epileptic seizure course and is a predictor of a disease nature as well as of an availability of comorbid psycho-emotional disorders. In particular, the presence of the first variant of the above clusters (the reduction in representing tracts in frontal brain regions) appeared to be typical for patients with drug-resistant forms of epilepsy (r = 0.46, p = 0.0005) (fig. 2). This cluster was typical for patients whose work was not notable for intellectual tension and who had no creative hobby (r = 0.39, p = 0.02), the disease began in early childhood (r = 0.53, p = 0.0001), the epiactivity on EEG was recorded bilaterally (r = 0.7, p < 0.0001) and there was an increase in the average amplitude of the theta rhythm (r = 0.58, p = 0.0003).
/16.jpg)
The reduced tract representation in external hemisphere parts correlated with the type of an epilepsy debut: a bilateral path «depletion» was typical for the onset of the disease in the form of a generalized tonic-clonic seizure, for a focal onset — a monolateral decrease in passer representing (r = 0.42, p = 0.03).
The absence of anterior and/or posterior commissures of cerebral hemispheres correlated to the latency of cognitive potential P300 (r = 0.39, p = 0.029). Comparing 1Н-МРС results to the data of diffusion tensor MRI has shown the relation of low NAA/(Cho + Cr) values in external temporal lobe parts with the absence of imaging brain anterior and/or posterior commissures (r = 0.8, p = 0.009) that demonstrates the significance of normal conditions of brain white matter passers for an adequate functioning of cortical regions.
Thus, the integrity of anterior and posterior brain commissures correlated with cognitive functions.
We revealed a correlation between the test results according to Beck scale and a pathological decrease in FA values (r = 0.11, p < 0.05) and an increase in MDC (r = –0.2, p < 0.01). The latent period Р300 correlated to the FA values of the frontal lobe of an epileptogenic hemisphere (r = 0.23, p < 0.001). The combination of the cluster of tractographic pattern depletion in frontal parts and the cluster of a decrease in imaging brain commissures is the most unfavorable one concerning the development of cognitive and psycho-emotional disorders in epilepsy (fig. 2).
The values of Spielberger-Khanin test both for trait and situational anxiety had a strong negative correlation with NAA/(Cho + Cr) parameters in external parts of a temporal lobe on the side of an epileptic focus (r > –0,7, p < 0,03) (fig. 3). NAA/(Cho + Cr) values in the hippocampus on a focus side correlated with the amplitude of the main peak N2-P3 of the induced cognitive potential P300 (r = 0.67, p = 0.047).
/17.jpg)
Studying the peculiarities of EEG-finding and FA values demonstrated a correlation between an epileptic activity and a decrease in FA (r = 0.7, t = 2.44, p = 0.01). Normal values of amplitude, frequency and alpha-rhythm index were typical of patients with unchanged FA parameters (p < 0.05). The alpha rhythm inversion (r = 0.44, t = 3.12, p = 0.0033) and the increase in a theta-rhythm index were accompanied by a FA decrease (r = 0.32, t = 2.15, p = 0.038). It should be noted that theta-rhythm flashes had no correlation with any of diffuse tensor MRI values. Finding a positive correlation of focusing theta rhythm and normal FA values (r = 0.27, p = 0.00001) suggests that the detection of this EEG phenomenon is characteristic of relatively intact brain structures that have the potential effectively to enable inhibitory mechanisms.
Thus, in patients with epilepsy compared to controls, we revealed the presence of discrete regions of anomalously changed brain white matter, with abnormalities localized not only in an epileptogenic hemisphere but in an opposite one.
Discussion
The FA value appeared to be more specific among DT MRI for detecting structural lesions, for prognosing a disease course — MDC and the «depletion» of a tract picture in external temporal lobe parts especially in the phenomenon of contralateral hippocampal deafferentation. The white matter regions with abnormal FA and MDC values were consistent with the zones of changed tracts not only of the limbic circle but with the zones of intra- and inter-hemispheric connections uniting frontal, temporal, parietal and occipital lobes of the brain.
The condition of brain commissures integrity provides the stability of cognitive and emotional status of a patient. Latent period P300 appeared to be the most sensitive one to the changes of brain white matter integrity among characteristics of mental functions that probably is a consequence of an abnormality of interhemispheric integral interaction provided by intact corpus callosum. Pathological changes in the EEG pattern in epilepsy are largely due to an abnormality of brain tracts integrity. Diffusion tensor MRI with tractography lets extend the conception of microstructural changes of gray and white matter integrity in epilepsy and define an etiological structural-metabolic subtype of this disease according to the recommendations of the International League against Epilepsy [1]. The results obtained showed that epilepsy is characterized by a variety of changes of brain white matter passers which lead to disconnecting certain brain areas that in its turn causes a further impairment of connections between cortical and subcortical parts and changes an information transmission. In particular, the absence of anterior and/or posterior commissures of the brain at tractography predicts subsequent development of a clinically significant cognitive impairment.
Conclusions
Diffusion tensor magnetic resonance imaging is an informative method of detecting structural brain lesions in patients with epilepsy. Using this method lets identify the presence of structural lesions in all the surveyed patients as well as quantify the fractional anisotropy and the mean diffusivity capacity of the structure of the white matter involved in an epileptic process. The distinction of specific clusters of brain tract lesions in epilepsy is important for prognosing a disease course and a probable possibility of cognitive abnormalities. The depletion of visualization or the absence of anterior and/or posterior brain commissures at diffusion tensor tractography predicts subsequent development of clinically significant cognitive abnormalities.
According to our results, psycho-emotional disorders in epilepsy are associated with neurometabolic disorders in external parts of brain temporal lobes. The reduction of the main peak amplitude P300, which is an objective characteristic of attention processes, correlates with metabolic process disorders in hippocampal structures.
The combination of the cluster of the tractographic picture depletion in frontal parts and the cluster of the reduction of imaging brain commissures is the most unfavorable one in relation to developing cognitive and psycho-emotional disorders in epilepsy.
Modern neuroimaging techniques provide an opportunity for pathogenic diagnosis, adding clinical criteria for epilepsy.
Disclosure Policy. The authors declare that there is no conflict of interest regarding this paper.
Acknowledgements
This work was performed in the context of the scientific research theme «The Regularities of the Anticonvulsive Action of Pulsed Magnetic Fields and Their Clinical Application» of the State Programs of the Scientific Research «Convergence» of the National Academy of Sciences of Belarus.
We are grateful to Natalya Plotnikova for the help in professional translating this article.

/15.jpg)
/16.jpg)
/17.jpg)