Журнал «Здоровье ребенка» Том 14, №2, 2019
Вернуться к номеру
Тахіаритмія в новонароджених. Клінічний випадок тріпотіння передсердь у новонародженого
Авторы: O.B. Kuryliak(1), T.V. Burak(2), A.A. Malska(3)
(1) — MI “Lviv Regional Children’s Hospital “OHMATDYT”, Lviv, Ukraine
(2) — Western Ukrainian Specialized Children’s Medical Center, Lviv, Ukraine
(3) — Danylo Halytskyi Lviv National Medical University, Lviv, Ukraine
Рубрики: Педиатрия/Неонатология
Разделы: Справочник специалиста
Версия для печати
Актуальність. Тахіаритмії — це найбільш небезпечне порушення ритму в новонароджених і дітей грудного віку. Рідкісною формою тахіаритмії, не характерною для новонароджених, є тріпотіння передсердь (ТП). ТП у новонароджених трапляється із частотою 1 : 50 000 та становить 3 % від усіх порушень ритму в новонароджених. Мета полягає у дослідженні тахіаритмії новонароджених на прикладі клінічного випадку тріпотіння передсердь у новонародженого. Матеріали та методи. У цій статті було розглянуто клінічний випадок складного порушення ритму в новонародженого хлопчика, а саме: тріпотіння передсердь 2 : 1, 3 : 1 із рецидивуючими приступами пароксизмальної надшлуночкової тахікардії, частими шлуночковими екстрасистолами та зниженою скоротливістю міокарда. Для дослідження тріпотіння передсердь було використано такі методи: ЕКГ, 2D допплер-ЕхоКГ. Результати. Медикаментозне лікування цього порушення ритму полягало в наступному: АТФ в/в болюсно, повторно — неефективно, інфузія кордарону 15 мг/кг/день, седація. У зв’язку з наростанням серцевої недостатності та низькою скоротливою здатністю міокарда було додано інотропну терапію (дигоксин 20 мкг/кг). У результаті синусовий ритм було відновлено протягом доби. Продовжено інфузію кордарону в дозі 10 мг/кг/день протягом 5 днів із переходом на 5 мг/кг/день. Таким чином, у динаміці за даними ЕхоКГ: зменшились розміри камер серця, внутрішньосерцевих аномалій не було виявлено. Кровотік у низхідній аорті пульсуючий, покращилась скоротлива здатність міокарда: ФВ зросла — 45–50–62–66 %. Більше того, на ЕКГ в динаміці спостерігалось відновлення синусового ритму з ЧСС 130 уд/хв, без ознак гіпертрофії міокарда й порушень провідності. Висновки. У нашому випадку лікування епізоду ТП новонародженого — відновлення синусового ритму — досягнуто шляхом медикаментозної терапії. Альтернативним методом лікування ТП у новонароджених є синхронізована електрична кардіоверсія 0,5–1,0 Дж/кг [5, 6].
Актуальность. Тахиаритмии — это наиболее опасное нарушение ритма у новорожденных и детей грудного возраста. Редкой формой тахиаритмии, не характерной для новорожденных, является трепетание предсердий (ТП). ТП у новорожденных встречается с частотой 1 : 50 000 и составляет 3 % от всех нарушений ритма у новорожденных. Цель заключается в исследовании тахиаритмии новорожденных на примере клинического случая трепетания предсердий у новорожденного. Материалы и методы. В этой статье был рассмотрен клинический случай сложного нарушения ритма у новорожденного мальчика, а именно: трепетание предсердий 2 : 1, 3 : 1 с рецидивирующими приступами пароксизмальной наджелудочковой тахикардии, частыми желудочковыми экстрасистолами и пониженной сократимостью миокарда. Для исследования трепетания предсердий были использованы следующие методы: ЭКГ, 2D допплер-ЭхоКГ. Результаты. Медикаментозное лечение данного нарушения ритма состояло в следующем: АТФ в/в болюсно, повторно — неэффективно, инфузия кордарона 15 мг/кг/сут, седация. В связи с нарастанием сердечной недостаточности и низкой сократительной способностью миокарда была добавлена инотропная терапия (дигоксин 20 мкг/кг). В результате синусовый ритм был восстановлен в течение суток. Продлена инфузия кордарона в дозе 10 мг/кг/сут в течение 5 дней с переходом на
5 мг/кг/сут. Таким образом, в динамике по данным ЭхоКГ: уменьшились размеры камер сердца, внутрисердечных аномалий не было обнаружено. Кровоток в нисходящем отделе аорты пульсирующий, улучшилась сократительная способность миокарда: ФВ возросла — 45–50–62–66 %. Более того, на ЭКГ в динамике наблюдалось восстановление синусового ритма с ЧСС 130 уд/мин,
без признаков гипертрофии миокарда и нарушений проводимости. Выводы. В нашем случае лечения эпизода ТП новорожденного —восстановление синусового ритма — достигнуто путем медикаментозной терапии. Альтернативным методом лечения ТП у новорожденных является синхронизированная электрическая кардиоверсия 0,5–1,0 Дж/кг [5, 6].
Background. Tachyarrhythmia is the most severe rhythm disturbance in pediatric population. Atrial flutter is an extremely rare form of tachyarrhythmia and is not typical for newborns. Incidence of atrial flutter in neonates is 1 : 50,000 and amounts 3 % out of all rhythm disturbances in neonates. The purpose was to present a clinical case of atrial fibrillation in a newborn and literature overview of the treatment of tachyarrhythmia in children of different age. Materials and methods. This article presents a clinical case of severe rhythm disturbance — atrial fibrillation 2 : 1, 3 : 1 with the recurrent episodes of supraventricular tachycardia, frequent ventricular ectopic beats and diminished ejection fraction in a newborn. The following diagnostic methods were used in the research: ECG and 2D Doppler echocardiography. Results. The following treatment was applied in this particular case: adenosine bolus i/v, second infusion — without effect, cordarone infusion 15 mg/kg/d, sedation. Due to the progression of heart failure and decrease of ejection fraction, inotropic therapy was started (digoxin 20 μg/kg). As a result, the sinus rhythm was restored within 24 hours. Infusion of cordarone 10 mg/kg was continued for the following 5 days with transition to 5 mg/kg dosage. Thereby, repeat echo-examination results showed heart chambers decreased in size, no intracardiac anomalies, pulsatile blood flow in the descending aorta and the ejection fraction improved to 45–50–62–66 %. As follows, sinus rhythm with the heart rate of 130 beats per minute was monitored without the signs of chambers hypertrophy and conduction disturbances. Conclusions. In this particular case, the treatment of atrial flutter episode — gaining the sinus rhythm was achieved by drug therapy. Alternative method of treatment is cardioversion 0.5–1.0 J/kg [5, 6].
тахіаритмії; новонароджений; діагностика; лікування
тахиаритмии; новорожденный; диагностика; лечение
tachyarrhythmia; newborn; diagnosis; treatment
Introduction
Tachyarrhythmia is the most severe rhythm disturbance in pediatric population. Atrial flutter (AF) is an extremely rare form of tachyarrhythmia and is not typical for newborns [1]. Literary sources demonstrate that AF incidence in neonates is 1 : 50 000 and amounts 3 % out of all rhythm disturbances in neonates [2, 3]. AF in most newborns manifest itself during the first 48 hours after the birth and can lead to heart failure, thromboembolism, arrhythmogenic cardiomyopathy or sudden death. The etiology of AF is insufficiently explored; it is believed that it can be caused by immaturity of the cardiac muscle and high blood pressure in the right atrium in the perinatal period [4]. It is also known that there is a relation between AF and such pathologies as cardiomyopathy, atrium tumors, infectious endocarditis, lymphangiectasia and endocardium fibroelastosis [4], congenital heart defects (hypoplasia of the left heart chambers, LA atresia, etc.). Following the research works of other authors, no substantial interrelation between AF occurrence and structural cardiac pathology has been found.
In one third of patients, tachyarrhythmia never repeats after the first year of life; however, heart failure in newborns develops more rapidly and depends upon its duration, mechanism and frequency of occurrence.
Atrial flutter is diagnosed with ECG: atrial contraction rate of more than 440 beats per minute is registered, mostly with 2 : 1, 3 : 1 atrioventricular contraction and F-waves in ІІ, ІІІ and aVF lead. Sometimes variable AV conduction and irregular ventricular contraction rate of 125 beats per minute are observed. Differential diagnosis should be performed with multifocal supraventricular and other forms of supraventricular tachycardia.
Clinically: tachyarrhythmia in infants manifests itself with such nonspecific symptoms, as: pallescence, difficulty in feeding, shortness of breath and excessive sweating, which as a rule are revealed during the objective pediatric examination.
AF is frequently diagnosed during the fetal echocardiography, when the atrial contraction rate of more than 400 beats per minute with conductivity 2 : 1 and ventricular contraction rate of 200 beats per minute are registered. The start of the episode in the fetal period is generally associated with the edema neonatorum. AF is clinically manifested with high heart rate and congestive heart failure.
Treatment of AF presupposes regaining a normal sinus rhythm. In accordance with literary sources, the fastest method of achieving this is applying synchronized cardioversion 0.5–1.0 J/kg. However, the newborn’s response to treatment can be variable and unpredictable.
Episodes of all types of tachyarrhythmia, except AF (at AF it is recommended to apply cardioversion [6]), in newborns should be treated initially with vagal maneuvers with subsequent bolus administration of adenosine [7, 8], nevertheless, there are abundant published research papers describing the efficacy of other antiarrhythmic remedies.
In 1998, F. Drago et al. [9] proposed an effective therapy for tachyarrhythmia in infants and children. The loading dose of amiodarone of 10–20 mg/kg/day and the maintenance dose of 3–20 mg/kg/day was used. After amiodarone came up short, propranolol 2–4 mg/kg/day was added. Children were randomized into two groups: group A consisted of the infants younger than 1 year of age and group B included children older than 1 year of age. The authors made conclusion that amiodarone is an effective remedy for the treatment of the refractory atrial and ventricular tachyarrhythmia, especially in children over 1 year of age. And its combination with propranolol substantially improves the efficacy of the treatment of atrioventricular reciprocating tachycardia in infants < 1 year old.
In 2017, the group of researchers from China published in the American Journal of Cardiology the new data regarding the use of injectable sotalol for the removal of tachyarrhythmia episodes in children [10].
The research group included 83 children, in 60 % of them the sinus rhythm was restored during 12 ± 18 hours with i/v sotalol infusion, and in 15 % with sotalol and propafenone infusion; the time till regaining the sinus rhythm amounted 13.0 ± 17.6 hours. In total, the sinus rhythm was restored in 62 (75 %) children after the i/v sotalol infusion. The authors reached the conclusion that children with supraventricular paroxysmal tachycardia regain the sinus rhythm sooner in comparison with children with atrial tachyarrhythmia and atrial fibrillation, and propafenone accelerates the sinus rhythm recovery.
In 2017, the same researchers published another article on intravenous sotalol dosage on the basis of the total body area index in patients with arrhythmias [11]. The research group included 83 patients, among them 5 newborns (age: 0–30 days), 39 infants (age: 1–24 months), 26 toddlers (age: 2–6 years), 11 older children (age: 6–12 years) and 2 teenagers (age: 14 years). Each of them received the loading dose of 1 mg/kg of i/v sotalol during 10 minutes with transition to the maintenance dose of 4.5 mg/kg/day. The apparent correlation was observed between the doses of accumulation calculated using the total body area index in all groups (r = 0.977; p = 0.001).
In 2013, the Pediatric Cardiology journal [12] published the research: “Verapamil in infants: an exaggerated fear?”. It is known that i/v verapamil for tachyarrhythmia treatment in newborns is considered counter-indicative as it bears high risk of causing hemodynamic collapse immediately after administration. The article analyzes the clinical cases of applying verapamil in infants.
The authors arrive at the conclusion that tachyarrhythmia treatment should be started with vagal maneuvers and adenosine. However, in the cases of focal ectopic atrial tachycardia or fascicular ventricular tachycardia it is recommended to apply calcium channel blockers at a dose of 0.1–0.2 mg/kg starting from the lowest one. Absence of effect from the increased dose indicates the necessity to discontinue the use of this drug. Additionally, verapamil should not be used together with digoxin. The episode should be removed with connecting the patient to the observation monitor.
In 2015, in the Journal of Pediatrics, Andrea L. Barton et al. published the article [13] about the efficacy and safety of high dosage propranolol for the treatment of supraventricular tachycardia in newborns. The research was held over 287 children with the average age of 17 days and with the average dose of 3.6 ± 1.0 mg/kg/day. In 67.3 % of patients the episode was successfully eliminated and treatment of only one patient had to be suspended due to occurrence of complications. Out of 190 children discharged after propranolol monotherapy, 87.7 % had no recurrent episodes of paroxysmal tachycardia. Thus, the authors made the conclusion that propranolol monotherapy in newborns is a safe and effective method for the elimination of paroxysmal tachycardia episodes in newborns.
In 2018, the Pediatric Cardiology journal [14] published the article of the Japanese researchers about the safety and efficacy of the usage of radiofrequency catheter ablation (RFA) for tachyarrhythmia in children with the weight less than 10 kg. The research group included 285 children, whom RFA was performed and who were subdivided into subgroups depending on the body weight. Group A included the children with the weight less than 10 kg (n = 22), and group B included the children with the weight over 10 kg, respectively (n = 263). The indications for applying ablation in these children included: refractory tachyarrhythmia, symptomatic tachycardia and cardiomyopathy due to tachyarrhythmia. The researchers describe the 90.9% level of successful tachyarrhythmia treatment with relatively low frequency of recurrence after 7.0 ± 1.6 years of observation. The scientists concluded that RFA in children with the weight less than 10 kg is completely safe and effective, and the rate of complications and repeated episodes is absolutely acceptable.
In accordance with the scientific research data published by various scientific centers, the life expectancy forecast for children with tachyarrhythmia, in particular in newborns with AF, is favorable so as no other tachyarrhythmia are diagnosed, and the risk of recurrence is extremely low and does not require any additional preventive measures.
The purpose was to study tachyarrhythmia in newborns on the example of the clinical case of atrial flutter in a newborn.
Materials and methods
This article describes a clinical case of the severe rhythm disturbance in a newborn boy, i.e. atrial flutter 2 : 1, 3 : 1 with the recurrent episodes of paroxysmal supraventricular tachycardia, frequent ventricular ectopic beats and reduced myocardial contractility. The following diagnostic methods were used in the research: ECG, fetal echocardiography and echocardiography.
Results
A newborn boy (date of birth: 24.04.2018) was transported to the neonatal intensive care unit of the Municipal Institution “Lviv Regional Children’s Hospital “OHMATDYT” in reanimobile on the first day of life with the episode of supraventricular paroxysmal tachycardia, heart rate — 220 beats per minute.
The anamnesis showed that the child was born after the full-term pregnancy (38th week of gestation), the 1st birth, by the caesarean section with the weight of 4400 g and the height 56 cm. Apgar score was 8/8 points. It is known that the mother was registered at the obstetric hospital starting from the 15th week of pregnancy. The obstetric history included complications, i.e. previous surgical treatment of the pituitary tumor, bronchial asthma and treatment with symbicort during the pregnancy. On the 25th week of the pregnancy, the mother had ARVI and the threat of miscarriage.
When hospitalized to the intensive care unit, the child’s condition was critical due to the respiratory and cardiovascular insufficiency. The skin cover was pale, the acrocyanosis was observed and the child was restless. The child was with the correct body structure and satisfactory nutritional status. The physical growth and development corresponded to the average level, was well-balanced, weight 4400 g, blood pressure 95/55 mmHg, heart rate 138–220 beats per minute, respiratory rate 45/minute, SpO2 90–97 %.
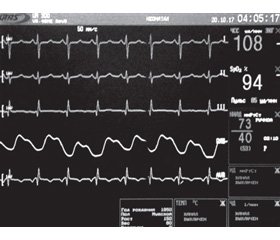
Course of the disease: during the first 2 days, the disturbance of the heart rhythm preserved, ECG showed frequent supraventricular ectopic beats, blocked supraventricular ectopic beats, grouped ventricular ectopic beats, episodes of atrial flutter with the contraction rate of 400–450 beats per minute being replaced with prolonged paroxysms of supraventricular tachycardia with narrow complexes (atrial flutter 2 : 1, 3 : 1) with the ventricular contraction rate of 220–138 beats per minute (Fig. 1–8).
Echocardiography revealed dilatation of both ventricles and both atria, restrictive oval window, arterial duct in the closure stage, hemodynamically irrelevant, no intracardiac anomalies detected; ejection fraction reduced to 40 %.
It was decided to apply pharmacological therapy for rhythm disturbance treatment: adenosine bolus i/v, second infusion — without effect, cordarone infusion
15 mg/kg/day, sedation. Due to the progression of heart failure and decrease of ejection fraction, inotropic therapy was started (digoxin 20 μg/kg).
As a result, the sinus rhythm was restored within 24 hours. Infusion of cordarone 10 mg/kg was prolonged for the following 5 days with transition to 5 mg/kg dosage.
Thereby in dynamics, according to echo-exam: heart chambers decreased in size, no intracardiac anomalies were identified, blood flow in the descending aorta was pulsatile and the ejection fraction improved to 45–50–62–66 %.
As follows, sinus rhythm with the heart rate of 130 beats per minute was monitored without the signs of chambers hypertrophy and conduction disturbances (Fig. 9).
The patient was discharged from hospital on the sixth day and the outpatient treatment was prescribed: digoxin 0.00002 once a day — 1 month, cordarone — 5 mg/kg/d for one month. In the age of one month, the Holter monitoring of ECG was performed: the basic rhythm — sinus, the heart rate — 120–130 beats per minute, sporadic atrial ectopic beats.
Recently the child reached 6 months of age and no recurrent episodes have occurred since that time.
Discussion
In research works, there are several clinical cases described when severe rhythm disturbances in newborns manifested in the form of atrial flutter without recurrent episodes in the long-term follow-up period, as distinguished by the authors. The issue of the therapeutic tactics for the treatment of supraventricular tachycardia and atrial flutter in newborns and infants still remains controversial. This is related to the small amount of researches substantiating the optimal therapeutic tactics taking into account the peculiarities of the pediatric application. The approaches to tachyarrhythmia treatment differ depending on the local protocols of various clinics [5–7]. Other research papers are published describing the efficacy of other antiarrhythmic remedies (propranolol, amiodarone, sotalol, verapamil [8–12]) and their combinations.
Conclusions
In this particular case, the treatment of AF episode — gaining the sinus rhythm was achieved by drug therapy. Alternative method of treatment is cardioversion 0.5–1.0 J/kg [5, 6].
Conflicts of interests. Authors declare no conflicts of interests that might be construed to influence the results or interpretation of their manuscript.
1. Shilpa K. Idiopathic Neonatal Atrial Flutter [Electronic resource] / K. Shilpa, N. Kanade, U. Pratap, S. Gupte // Ped. Oncall. — 2016. — Vol. 13. — Mode of access: https://www.pediatriconcall.com/pediatric-journal/view/fulltext-articles/1011/J/0/0/536/0. doi: 10.7199/ped.oncall.2016.14.
2. Mode of access: https://www.orpha.net/consor/cgi-in/OC_Exp.php?Lng=GB&Expert=45452.
3. Sivakumar S. Atrial flutter in preterm babies [Electronic resource] // BMJ Journals. — 2004. — Mode of access: https://fn.bmj.com/content/89/6/F564.
4. Estlin E.J. Atrial fibrillation with neonatal pulmonary lymphangiectasia / E.J. Estlin, M.K. Bennett, J.R. Skinner, D.W. Milligan, C. Wren // Acta Paediatr. — 1998. — Vol. 87. — P. 1304-6. doi: 10.1111/j.1651-2227.1998.tb00957.x.
5. Tunca G. Evaluation of Sustained Tachyarrhythmia in Children Younger Than One Year of Age [Electronic resource] / G. Tunca, S. Erkut, O. Erkut, O. Taner, K.A. Guzeltas, Y. Ergul. — 2017. — Mode of access: https://doi-org.proxy-um.researchport.umd.edu/10.1111/ped.13445. doi: 10.1111/ped.13445.
6. Siromaka S.O. The case of emergency treatment of atrial flutter in the newborn / S.O. Siromaka, L.M. Prokopovych, V.P. Zalevskyi et al. // Ukrainian Cardiology Journal. — 2016. — 6. — P. 112-114.
7. Vukomanović V. Neonatal supraventricular tachyarrhythmias: Analysis of treatment efficacy and therapeutic approach recommendations / V. Vukomanović, J. Košutić, S. Ninić et al. // J. Perinat. Med. — 2017. — Vol. 45. — P. 302-303.
8. Richardson Ch. Management of Supraventricular Tachycardia in Infants / Ch. Richardson, E.S. Silver // Pediatric Drugs. — 2017. doi: 10.1007/s40272-017-0254-0.
9. Drago F. Amiodarone Used Alone or in Combination with Propranolol: A Very Effective Therapy for Tachyarrhythmias in Infants and Children / F. Drago, A. Mazza, P. Guccione, A. Mafrici, G. Di Liso, P. Ragonese // Pediatr. Cardiol. — 1998. — Vol. 19. — Р. 445-449.
10. Li X. Efficacy of intravenous sotalol for treatment of incessant tachyarrhythmias in children / X. Li, Y. Zhang, H. Liu, H. Jiang, H. Ge, Y. Zhang // Am. J. Cardiol. — 2017. — Vol. 119. — P. 1366-1370.
11. Li X. Pediatric Dosing of Intravenous Sotalol Based on Body Surface Area in Patients with Arrhythmia / X. Li, Y. Zhang, H. Liu, H. Jiang, H. Ge, Y. Zhang // Pediatr. Cardiol. — 2017. — Vol. 38. — P. 1450-1455.
12. LaPage M.J. Verapamil in Infants: An Exaggerated Fear? / M.J. LaPage, D.J. Bradley, M. Dick // Pediatr. Cardiol. — 2013. — Vol. 34. — P. 1532-1534.
13. Barton A.L. Efficacy and safety of high-dose propranolol for the management of infant supraventricular tachycardia [Electronic resource] / A.L. Barton, B.S. Hoffet, S.O. Valdes, Ch. Miyake, J.J. Kim // Journal of pediatrics. — 2015. — Mode of access: http://dx.doi.org/10.1016/j.jpeds.2014.08.067.
14. Ozaki N. Safety and Efficacy of Radiofrequency Catheter Ablation for Tachyarrhythmia in Children Weighing Less Than 10 kg [Electronic resource] / N. Ozaki, Y. Nakamura, T. Suzuki et al. // Pediatr. Cardiol. — 2018. — Vol. 39. — P. 384-389. — Mode of access: https://doi.org/10.1007/s00246-017-1766-7.
15. 4 Oral Presentations [Electronic resource] / J. Perinat. Med. — 2017. — Vol. 45. — Iss. s2. — P. 276-422. — Mode of access: doi: https://doi.org/10.1515/jpm-2017-2008.

/107-1.jpg)
/108-1.jpg)
/108-2.jpg)
/108-3.jpg)