Международный неврологический журнал №8 (110), 2019
Вернуться к номеру
Наслідки таламічних інсультів: проспективне клінічне когортне дослідження
Авторы: S.M. Vinychuk(1), M.M. Prokopiv(2), L.M. Trepet(1), O.Ye. Fartushna(3)
(1) — Oleksandrivska Clinical Hospital, Kyiv, Ukraine
(2) — Bogomolets National Medical University, Kyiv, Ukraine
(3) — Ukrainian Military Medical Academy, Kyiv, Ukraine
Рубрики: Неврология
Разделы: Клинические исследования
Версия для печати
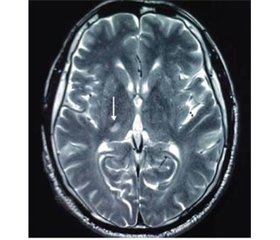
Актуальність. Інсульт є другою за частотою причиною смертності у світі, поступаючись лише смертності від серцево-судинних захворювань. Проте на сьогоднi опубліковано недостатньо прoспективних клінічних досліджень, у яких описані й проаналізовані клінічні характеристики та наслідки таламічних інсультів. Мета дослідження: визначити особливості наслідків гострого таламічного інсульту в проспективному клінічному когортному дослідженні, забезпечивши всебічний клінічний і нейровізуалізаційний аналіз результатів лікування та наслідків гострого таламічного інсульту. Матеріали та методи. Ми провели проспективне клінічне когортне дослідження 319 пацієнтів iз гострим ішемічним інсультом, які надійшли до неврологічного центру Олександрівської клінічної лікарні (м. Київ, Україна) протягом перших 24 годин з моменту розвитку хвороби. Усі пацієнти пройшли комплексне клініко-неврологічне, лабораторне, ультразвукове та ней-ровізуалізаційне обстеження. Результати. Серед 319 хворих iз гострим ішемічним інсультом нейровізуалізаційно підтверджений таламічний інсульт діагностовано в 34 (10,6 %) ocіб: у 22 (середній вік 61,9 ± 10,2 року) виявлено гострий ізольований інфаркт таламусу, а в 12 пацієнтів (середній вік 59,0 ± 9,6 року) — гострий таламічний крововилив. Описані, проаналізовані та порівняні клінічні наслідки інфарктів різних таламічних територій.
Актуальность. Инсульт является второй по частоте причиной смертности в мире, уступая лишь смертности от сердечно-сосудистых заболеваний. Тем не менее в настоящее время опубликовано недостаточно проспективных клинических когортных исследований, в которых описаны и проанализированы клинические характеристики и последствия таламических инсультов. Цель исследования: определить особенности исходов острого таламического инсульта в проспективном клиническом когортном исследовании, обеспечив всесторонний клинический и нейровизуализационный анализ результатов лечения и исходов острого таламического инсульта. Материалы и методы. Мы провели проспективное клиническое когортное исследование 319 пациентов с острым ишемическим инсультом, поступивших в неврологический центр Александровской клинической больницы (г. Киев, Украина) в течение первых 24 часов с момента развития болезни. Все пациенты прошли комплексное клинико-неврологическое, лабораторное, ультразвуковое и нейровизуализационное обследования. Результаты. Среди 319 больных с острым ишемическим инсультом нейровизуализационно подтвержденный таламический инсульт диагностирован у 34 (10,6 %) пациентов: у 22 (средний возраст 61,9 ± 10,2 года) выявлен острый изолированный инфаркт таламуса, а у 12 пациентов (средний возраст 59,0 ± 9,6 года) — острое таламическое кровоизлияние. Описаны, проанализированы и сравнены клинические последствия инфарктов различных таламических территорий.
Background. Stroke is the second-leading global cause of death behind heart disease, accounting for 11.8 % of total deaths worldwide. However, currently, there are not enough published prospective hospital-based cohort studies that report and analyze outcomes of thalamic stroke. The purpose of this study is to determine the features of acute thalamic stroke outcomes in a prospective hospital-based cohort study, providing a comprehensive clinical and neuroimaging analysis of the treatment results and assessing the outcomes of acute thalamic stroke. Materials and methods. We prospectively recruited 319 acute stroke patients, admitted within 24 hours from the onset of the stroke symptoms to the Neurological Center at an academic hospital (Oleksandrivska Clinical Hospital) in Kyiv, Ukraine. Comprehensive neurological, clinical, laboratory, ultrasound, and neuroimaging examination was performed in all patients. Results. MRI/CT-proven thalamic stroke was diagnosed in 34 (10.6 %) out of 319 persons, forming a study group: 22 patients (average age 61.9 ± 10.2 years) were diagnosed with an acute isolated ischemic thalamus infarction; 12 (average age 59.0 ± 9.6 years) — with an acute thalamic hemorrhage. Specific neurological outcomes of infarctions and hemorrhages in different thalamic territories were analyzed, compared, and described.
таламус; інсульт; таламічний інсульт; ішемічний інсульт; крововилив; наслідки інсульту
таламус; инсульт; таламический инсульт; ишемический инсульт; кровоизлияние; последствия инсульта
thalamus; stroke; thalamic stroke; ischemic stroke; hemorrhage; stroke outcomes
Introduction
Materials and methods
Results and discussion
Conclusions
1. Benjamin E.J., Muntner P., Alonso A. [et al.]. On behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics — 2019 update: a report from the American Heart Association. Circulation. 2019. Vol. 139(10). P. e56-e528.
2. Johnson W., Onuma O., Owolabi M., Sachdev S. Stroke: a global response is needed. Bulletin of the World Health Organization. 2016. Vol. 94. P. 634-634A.
3. Vinychuk S.M., Fartushna O.Ye. Cerebrospinal and commissu-ral diaschisis in acute stroke patients: case analysis. Международный неврологический журнал. 2018. № 5(99). С. 20-25.
4. Fartushna O.Ye., Vinychuk S.M. Brain injury in patients with acute TIA: clinical features in different TIA subtypes. Международный неврологический журнал. 2017. № 3(89). С. 13-18.
5. Feigin V.L., Norrving B., Mensah G.A. Global burden of stroke. Circulation Research. 2017. Vol. 120(3). Р. 439-448.
6. Global Health Estimates. Geneva: World Health Organization, 2012. Режим доступу до журналу: http://www.who.int/healthinfo/global_burden_disease/en/
7. Lees R., McGrane F., Fartushna O., Broomfield N.M., Quinn T.J., Dani K., Forbes K., Dawson J. Vascular cognitive impairment/vascular dementia. The pattern of cognitive impairment in stroke survivors with carotid stenosis. International Journal of Stroke. 2014. № 9. P. 323-324.
8. Owolabi M.O., Akarolo-Anthony S., Akinyemi R. [et al.]. The burden of stroke in Africa: a glance at the present and a glimpse into the future / Cardiovasc. J. Afr. 2015. Vol. 26(2). Suppl. 1. P. S27-38.
9. Wilkins E., Wilson L., Wickramasinghe K. [et al.]. European cardiovascular disease statistics 2017. Brussels: European Heart Network, 2017. 188 p.
10. World Stroke Organization. Global Stroke Fact Sheet. 26.02.2019. Режим доступу до журналу: https://www.world-stroke.org/images/WSO_Global_Stroke_Fact_Sheet_final.pdf
11. Віничук С.М., Прокопів М.М. Гострий ішемічний інсульт. Київ: Наукова думка, 2006. 286 с.
12. Віничук С.М., Фартушна О.Є. Рання реабілітація після гострих ішемічних порушень мозкового кровообігу. Міжнародний неврологічний журнал. 2016. № 8(86). С. 34-39.
13. Евтушенко С.К., Филимонов Д.А., Евтушенко И.С. Новые факторы риска развития инсульта у лиц молодого возраста. Журнал неврологии и психиатрии им. С.С. Корсакова. Спецвыпуск. 2015. Т. 115. № 12. С. 3-12.
14. Фартушна О.Є., Прокопів М.М. Актуальність проблеми цереброваскулярних захворювань, транзиторних ішемічних атак та вдосконалення їх діагностики в системі охорони здоров’я в Україні. Проблеми військової охорони праці: [зб. наук. праць Української військово-медичної академії / за ред. проф. Білого В.Я.]. Київ: УВМА, 2007. Вип. 19. С. 335-342.
15. Фартушна О.Є., Віничук С.М. Виявлення та усунення васкулярних чинників ризику — важливий напрямок первинної профілактики транзиторних ішемічних атак та/чи інсульту. Український медичний часопис. 2015. № 1(105). С. 23-27.
16. Фартушна О.Є., Віничук С.М. Транзиторні ішемічні атаки. Київ: ВД «Авіцена», 2014. 216 с.
17. Feigin V.L., Nguyen G., Cercy K. [et al.]. GBD 2016 Lifetime Risk of Stroke Collaborators. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N. Engl. J. Med. 2018. Vol. 379(25). P. 2429-2437.
18. Institute for Health Metrics and Evaluation (IHME). Findings from the Global Burden of Disease Study 2017. Seattle, WA: IHME, 2018.
19. World Stroke Organization. Facts and Figures about Stroke. Режим доступу до журналу: http://www.world-stroke.org/component/content/article/16-forpatients/84-facts-and-figures-about-stroke
20. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017. Vol. 390(10100). Р. 1151-1210.
21. Wang H., Naghavi M., Allen C. [et al.]. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016. Vol. 388(10053). P. 1459-1544.
22. Фартушна О.Є., Віничук С.М. Епідеміологія транзиторних ішемічних атак в структурі гострих порушень мозкового кровообігу в Україні та інших країнах. Міжнародний неврологічний журнал. 2017. № 5(91). С. 105-111.
23. Bogousslavsky J., Donnnan G.S., Norrving B., Bamford J.M. Thalamic infarcts, lacunar and other subcortical infarctions. Oxford University Press, 1995. P. 149-170.
24. Виничук С.М., Ялынская Т.А., Виничук И.С. Инфаркты в вертебробазилярном бассейне: клиника и диагностика. Международный неврологический журнал. 2005. № 3. C. 13-21.
25. Lopez-Serna R., González-Colrmona P., López-Martinez M.J. Bilateral thalamic stroke due to occlusion of the artery of Percheron in a patient with patent foramen a vale: a case report. Med. Case Reports. 2009. Vol. 3. P. 7392.
26. Bogousslavsky J., Regli F., Uske A. Thalamic infarcts: clinical syndromes, etiology, and prognosis. Neurology. 1988. Vol. 38(6). P. 837-48.
27. Cheng H., Tian Y., Hu P., Wang J., Wang K. Time-based prospective memory impairment in patients with thalamic stroke. Behavioral Neuroscience. 2010. Vol. 124(1). P. 152-158.
28. Steinke W., Sacco R.L., Mohr J.P. [et al.]. Thalamic stroke. Presentation and prognosis of infarcts and hemorrhages. Arch. Neurol. 1992. Vol. 49. P. 703-710.
29. Виничук С.М., Прокопив М.М., Трепет Л.Н. Изолированный инфаркт таламуса: клинические синдромы, диа-гностика, лечение и исход. Український медичний часопис. 2012. № 2. С. 87-93.
30. Виничук С.М., Прокопив М.М., Трепет Л.Н. Таламические инсульты. Киев: Агат-Принт, 2018. 91 с.: ил. Библиогр.: с. 82-91.
31. Прокопів М.М., Трепет Л.Н. Крововилив у таламус: клінічні прояви, діагностика, лікування та наслідки. Український медичний часопис. 2018. № 6(2) (128). С. 1-4.
32. Kernan W.N., Ovbiagele B., Black H.R. [et al.]. Guidelines for the prevention of stroke in patients with stroke and transient ische-mic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014. Vol. 45. Р. 2160-2236.
33. Aho K., Harmsen P., Hatano S. [et al.]. Cerebrovascular di-sease in the community: results of a WHO collaborative study. Bull. World Health Organ. 1980. Vol. 58. P. 113-130.
34. Adams H.P., Bendixen B.H., Kappelle L.J. [et al.]. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke.1993. Vol. 24. P. 35-41.
35. Ringleb P., Schellinger P.D., Hacke W. [et al.]. [European Stroke Organisation 2008 guidelines for managing acute cerebral infarction or transient ischemic attack. Part 1]. Der Nervenarzt. 2008. Vol. 79. P. 936-957.
36. Adams R., Albers G., Alberts M. [et al.]. Update to the AHA/ASA Recommendations for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack. Stroke. 2008. Vol. 39. P. 1647-1652.
37. Fartushna O.Y. Emergency therapeutic approach as a secon-dary prevention of an acute ischemic stroke in patients with TIA. XX World Neurological Congress, 12–17.11.2011. Marrakesh, Morocco, 2011. P. 167.
38. Fartushnaya E.E., Vinichuk S.M. Reducing the risk of recurrent ischemic stroke, after transient ischaemic attack along with neuroprotective and antiaggregant therapy. XIV International Congress of Rehabilitation Medicine and immunorehabilitation, 16–21.10. 2009: abstract. Tel-Aviv, Israel, 2009. Р. 67.
39. Віничук С.М., Фартушна О.Є. Диференційоване лікування транзиторних ішемічних атак — ефективний спосіб профілактики повторних гострих церебральних подій. Міжнародний неврологічний журнал. 2014. № 6. С. 87-92.
40. Віничук С.М., Фартушна О.Є. Аторвастатин та його роль у профілактиці та лікуванні ішемічних порушень мозкового кровообігу. Здоров’я України. Київ, 2015. № 9. С. 3.
41. Фартушна О.Є., Віничук С.М. Використання оптимальної дози препарату Торвакард — важливий напрямок зниження ризику розвитку повторних транзиторних ішемічних атак та/чи інсульту. Семейная медицина. 2015. № 3. С. 223-227.
42. Віничук С.М., Фартушна О.Є. Рання реабілітація після гострих ішемічних порушень мозкового кровообігу. Міжнародний неврологічний журнал. 2016. № 8(86). С. 34-39.
43. Віничук С.М., Фартушна О.Є. Освітні програми профілактики транзиторних ішемічних атак та/чи інсульту. Український медичний часопис. 2014. № 5. С. 49-51.
44. Фартушна О.Є., Віничук С.М. Модифікація поведінкових чинників ризику як складова первинної профілактики транзиторних ішемічних атак та/чи інсульту. Український медичний часопис. 2014. № 6(104) — XІ/XІІ. С. 42-44.
45. Фартушна О.Є. Патогенетичні підтипи транзиторних ішемічних атак: особливості неврологічної клініки, гемодинаміки та лікування [Текст]: дис... канд. мед. наук: 14.01.15 / Фартушна Олена Євгенівна; Нац. мед. ун-т ім. О.О. Богомольця. Київ, 2012. 217 арк.: рис., табл. Бібліогр.: арк. 187-217.
46. Charlson M.E., Pompei P., Ales K.L. [et al.]. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 1987. Vol. 40(5). P. 373-385.
47. Brainin M., Bornstein N., Bousen G., Demarin V. Acute neurological stroke care in Europe: results of the European Stroke Care Inventory. Eur. J. Neurol. 2000. Vol. 7. P. 5-10.