Introduction
Children born with a gestational age of less than 37 weeks are considered preterm newborns1. Premature birth is caused by a diversity of factors and leads to respiratory, heart, motor, and metabolic disorders due to the immaturity of body organs. When intrauterine development is interrupted, premature children lose the containing protection of the womb and do not have the physiological maturity to counteract the force of gravity. Consequently, these infants adopt an extended position when in dorsal decubitus, which further hinders adaptation to the environment2, 3.
There has been an increase in the survival rate of premature infants at neonatal intensive care units (NICUs), but these children are submitted to diverse interventions that have harmful effects, such as stress, pain, and exposure to both ambient noise and light, causing further clinical instability. The positioning of a preterm newborn is a highly beneficial non-pharmacological intervention when performed properly and makes up part of neuroprotective care. In contrast, inadequate positioning can increase stress and pain as well as delay neuromotor development4.
Proper positioning and the changing of decubitus has a series of benefits, such as the promotion of the adequate alignment of the body to the midline, improvements in lung function, the ventilation/perfusion ratio, motor development, and the flexor pattern, the prevention of muscle shortening, a reduction in stress and pain, the regulation of behavioral and sleep/awake states, and the adequate experience of gravitational pressure on the joints and muscles, facilitating coordinated, more symmetrical movements. Compared to the intrauterine environment, however, positioning does not provide all the sensory experiences necessary for adequate development, such as the vestibular experience. Thus, the hammock method can be employed3, 5.
The hammock method involves tying the corners of the fabric to the corners of the incubator, simulating intrauterine containment and movements to enable postural organization, harmonization of movements, as well as reductions painful stimuli and energy expenditure. This is a humanized care strategy to enhance comfort and neuroprotection5, 6.
The benefits of the hammock method are reported in the literature and there has been increasing use of this method for preterm newborns at NICUs. This technique improves the sleep/awake state, behavior, and both motor and respiratory development while minimizing the negative effects of physical handling, increasing the survival rate, and shortening the stay in the NICU3. The aim of the present study was to perform a qualitative (systematic) and quantitative (meta-analysis) evaluation of the effects of the hammock method on pain/stress, vital signs, and behavioral state in preterm newborns.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were used to report the review process. Studies that evaluated the impact of the hammock method on preterm newborns in the NICU published since the inception of the databank were identified. The published protocol can be accessed through the PROSPERO registry (CRD 42020187600). The quality of the evidence was appraised using the GRADE approach to determine the strength of the results and conclusions.
Search strategy
Searches were conducted in the Cochrane, Embase, SciELO, LILACS, PEDro, PubMed, and Scopus databases for clinical studies comparing the hammock method to other methods for preterm newborns. Searches were conducted between October 2019 and July 2020 by two independent researchers using the following combination search terms: “Hammock positioning” OR “patient positioning” OR “Hammocks” OR “Hammock” OR “Rede de Descanso”. After the reading of the titles and abstracts, only articles reporting randomized, controlled, clinical trials and quasi-experimental studies conducted in the NICU with preterm newborns using the Hammock method as the main intervention were included. No restrictions were imposed regarding the date of publication (Fig. 1).
Eligibility criteria
Articles that met the inclusion criteria were read in full and the following data were extracted: title, author, year of publication, study design, outcomes, and main results. Articles that did not adequately specify the intervention and those with no information on the outcomes of interest were excluded.
Appraisal of risk of bias
The risk of bias of the selected articles was appraised with the aid of the PEDro tool. The following items were considered: eligibility criteria, randomized allocation, allocation concealment, compatibility of baseline data, blinding of patients, blinding of therapists, blinding of evaluators, adequate follow-up (acceptable loss up to 20 %), intention-to-treat analysis, inter-group comparison, point estimates and variability.
Ongoing studies
The following five randomized studies were ongoing:
Electromyographic Activity of Preterm Newborns Submitted to Hammock Positioning Brasília, DF — BRAZIL A randomized, clinical trial with the aim of analyzing the effects on electromyographic activity in premature newborns placed in a hammock compared to premature newborns not placed in this position with evaluations before and after the intervention. Predicted completion: Oct. 2017. https://ichgcp.net/clinical-trials-registry/NCT02668107
Hammock Positioning’s Influence on the Electromyographic Activity in the Flexor Muscles in Newborn Preterm Recife, PE — BRAZIL Randomized, double-blind study with 20 premature infants with the aim of analyzing the influence of hammock positioning in the incubator on muscle tone through the Dubowitz neurological examination and electrical activity of the rectus abdominis, biceps, and hamstring muscles through electromyography approximately 8 hours during the day for two days with three evaluations. Predicted completion: Jun/2016. https://clinicaltrials.gov/ct2/show/NCT02621996
Effects of Hammock Method in incubator on pain, sleep state and heart rate of premature newborns admitted to the Neonatal Intensive Care Unit — Pelotas, RS — BRAZIL. Randomized, controlled, triple-blind trial with the aim of assessing the effect on pain and sleep after positioning the infant in a therapeutic hammock for 30 minutes twice per day (morning and afternoon) in the intervention group (G2, n = 5). The control group (G1) was only observed while remaining in the heated incubator (n = 6). Predicted completion: 30/10/2017. UTN number: U1111-1209-1721. https://apps.who.int/trialsearch/Trial2.aspx?TrialID=RBR-8m8v2x
Effectiveness of using networks on reducing pain and improving sleep in premature — Curitiba, PR, BRAZIL — Randomized, controlled study to determine effect of hammock positioning on the reduction in pain and improvement in sleep/awake state of preterm newborns through pain (PIPP) and sleep/awake (adapted Brazelton scale) assessment scales divided into two groups with 25 participants each with duration of 120 minutes per day for five days. Predicted completion: 20/11/2017. UTN number: U1111-1179-6533. http://www.ensaiosclinicos.gov.br/rg/RBR-8s8c8c/
Hammock position and nesting in premature babies: a comparative study — Brazil, DF — BRAZIL. Randomized, crossover study with two arms and 20 premature participants with the aim of assessing better sleep quality of premature infants when in hammocks. The method developed by Prechtl (1974) was used for the assessment of sleep, which attributes scores to sleep/awake states: deep sleep = 1, active sleep = 2, sleepiness = 3, quite alert = 4, active alert = 5, crying = 6. Predicted completion: 11/03/2016. UTN number: U1111-1181-1309. https://apps.who.int/trialsearch/Trial2.aspx?TrialID=RBR %E2 %80 %9047hfqm
Meta-analysis strategy
The measures of the effects of treatment were performed using the RevMan program. Continuous data were analyzed using the mean difference and 95% confidence intervals (CIs) were reported for all estimates. Fixed effects or random effects models were used, depending on statistical heterogeneity. Moreover, the generic inverse variance method was used to combine controlled trials into a single meta-analysis.
Heterogeneity of the data was evaluated using forest plots of the effects of treatment reported by the individual studies and combined with heterogeneity among the studies. Heterogeneity was quantified using the I2 statistic and classified as without heterogeneity (less than 25 %), low heterogeneity (25 % to 49 %), moderate heterogeneity (50 % to 75 %), or substantial heterogeneity (greater than 75 %), as recommended by the Cochrane Collaboration. When there was evidence of apparent or moderate to substantial heterogeneity (I2 higher than 50 %), the possible causes were evaluated searching for evidence of bias or methodological differences among the trials.
Results
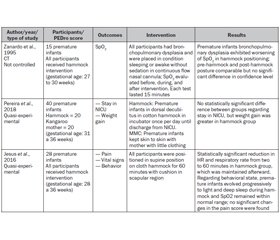
After the analysis of the eligibility of the articles retrieved during the searches of the databases, eight composed the final sample of the present systematic review, five of which were crossover studies. The studies involved samples of 15 to 40 premature infants (gestational age: 27 to 36 weeks) submitted to the hammock method. Five studies compared the hammock and nest methods (Table 1) and three compared the hammock method to other techniques, such as “kangaroo mother” (Table 2). Daily interventions were performed ranging from 15 minutes to three hours per day. The infants were placed in lateral decubitus in one study and in the supine position in all other studies. The primary outcomes were pain, behavioral state, and vital signs.
Studies included
Eight clinical trials were included in the present review, only three of which were randomized. The articles reported one or more of the outcomes of interest defined in the protocol of the present systematic review. Three were parallel studies and five were crossover studies.
Summary of articles included in the present review:
Sample size: 15 to 40 preterm newborns;
Inclusion criteria: gestational age 27 to 36 weeks and preterm newborns submitted to hammock method in NICU;
Recruitment time: Table 1.
Quantitative analysis
After the establishment of similarities among the results of the randomized clinical trials, four significant outcomes related to the hammock method were selected: heart rate (HR), Brazelton’s Neonatal Behavioral Assessment Scale (NBAS), pain assessment (Neonatal Facial Coding System [NFCS]), and peripheral oxygen saturation (SpO2).
Heart rate
Three studies composed the quantitative analysis of HR, with a total of 53 patients in the hammock group and nest group. No statistically significant difference in this outcome was found between groups.
Brazelton’s Neonatal Behavioral Assessment Scale
For the NBAS, 43 patients were in the hammock and nest groups. The hammock method achieved better results regarding behavioral state (Fig. 2).
Pain assessment
For the NFCS, 33 patients were in the hammock and nest groups. The pain score was lower in the hammock group compared to the nest group (Fig. 3).
Oxygen saturation
For SatO2, 53 patients were in the hammock and nest groups. The forest plot shows no statistically significant difference between groups for this outcome.
Risk of bias in studies
The risk of bias was appraised using the PEDro scale. The scores ranged from 3 to 7 points (out of a total of 10). Among the clinical trials, two were non-randomized, three were randomized, one was non-controlled, and three were quasi-experimental. The risk of bias was due to the non-blinding of the subjects and therapists. Only two studies involved blinded evaluators. Two studies had losses during follow-up. Four studies presented baseline data. Two studies did not perform inter-group comparisons (Table 3).
Discussion
The use of a hammock in the premature infant incubator achieves better results in comparison to other decubitus positioning methods, especially the nest method, with regards to pain and neuromotor behavior outcomes.
The participants were in the NICU in all studies included in the present review2, 3, 6–12. The exclusion criteria in most studies were hemodynamic instability2, 6, brain anomalies and neurological disorders2, 8, 9, > Grade II peri-intraventricular hemorrhage10, 12, apnea, fracture, having undergone painful procedures in the previous hour8, 9, congenital and facial malformations2, 6, congenital heart disease8, 10, 12, being on ventilatory support2, 8, 9, phototherapy, being in the immediate postoperative period, having received a surfactant in the previous 72 hours, and undergoing continuous sedation12. These exclusion criteria may have been established to avoid secondary events during the course of the interventions.
Preterm newborns undergo diverse procedures in the NICU that cause pain and stress, which are associated with morbidity and can have a long-term negative impact on numerous aspects13, 14. The studies in the present review assessed the pain outcome in this population2, 6, 12. Comparing the hammock method to prone positioning, Queiroz et al. found that both interventions were beneficial with regard to pain and vital signs2. In another study12, which analyzed the hammock method with no comparison to any other intervention, the authors found no change in pain scores among the premature infants, but reported that not having a control group constituted a limitation of the study. Ribas et al.6 analyzed pain comparing the hammock and nest methods in premature infants in lateral decubitus, concluding the that use of non-pharmacological methods, such as a hammock, relieves pain, promotes clinical stability, and improves homeostasis.
The tactile threshold and inhibitory pathways are immature in premature infants, making them more sensitive to pain13. Responses to pain stimuli begin in peripheral nociceptive pathways that manifest with spontaneous movements generated by the processing of this stimulus in the cortex. Nociceptors respond to mechanical, thermal, and chemical stimuli after the birth of the child and undergo changes with age. However, this modulation of nociceptive inputs occurs in the spinal cord. At the onset of development in preterm newborns, there is excessive excitation and a delay in the development of local descending inhibition, which generates a neonatal spinal reflex with a very low threshold, meaning that the reflex response is evoked by a less intense stimulus15.
Neonatal pain is directly associated with the repetitive stress to which premature infants are exposed in the NICU due to procedures and handling13, 16, which should be minimized in the first 72 h of life to avoid injuries and hemorrhages17. Moreover, premature birth deprives the infant of a contained, flexor position with vestibular stimuli in a fluid medium3. The less developed motor system has to overcome the gravity of the environment, which hinders adequate positioning8. The maintenance of a proper position provides control of the sleep/awake state and self-regulation, improves cardiorespiratory function, and requires less energy expenditure, resulting in lower stress8.
In preterm newborns, muscle tone evolves from a global state of hypotonus to hypertonus. The onset of flexion occurs with the increase in age — always in the caudocranial direction, with the flexors developing later than the extensors. The capacity of the newborn to adapt to the environment can be evaluated though spontaneous movements, which are facilitated by adequate positioning18.
The state of behavioral organization was evaluated by disorganized infant behavior in the study by Costa et al. (2016)8, which is based on synactive theory considering five subsystems: autonomic/physiological, regulation problems, attention/interaction system, organization system, and behavioral state/motor system. These are key aspects of neonatal self-regulation and interactions between the newborn and the environment19. Keller et al. also found evidence of synactive theory and associated it with findings of greater neuromuscular maturity in premature infants when placed in a hammock, demonstrating the importance of position in the development of the central nervous system in this population3.
The development of the central nervous system is divided into six steps: neurulation, prosencephalic development, neural proliferation, neuronal migration, organization, and myelinization. This organization has a peak period around the fifth month of gestation. When a premature infant grows in the NICU, this environment induces impactful changes in the brain development pattern. Thus, neuroprotective care strategies are important and lead to positive results with regards to neurological development. Newborn individualized development care (NIDC) is based on seven principal measures (represented by lotus petals): healing environment in partnership with the family, positioning and handling, safeguarding sleep, minimizing stress and pain, protecting skin, and optimizing nutrition20.
One of the aims of the present systematic review was to determine the effect of the hammock method on the vital signs of premature infants. Seven studies included in the review2, 3, 6, 9, 10, 12 evaluated this outcome. In five of these studies2, 3, 9, 10, 12, the infants were in the supine position in the hammock. Keller et al.3 found reductions in HR and respiratory rate associated with a more relaxed condition when in the hammock. Jesus et al. also found a significant reduction in HR and respiratory rate, with the maintenance of SpO2 at normal levels12. Zanardo et al. only investigated SpO2 in 15 premature infants, all of whom had a diagnosis of bronchopulmonary dysplasia and exhibited a worsening of SpO2, with no significant difference in the pre-hammock/post-hammock comparison10. Costa et al. (2019) also found no significant difference in vital signs. In contrast, Ribas et al.6 found a reduction in HR and respiratory rate as well as an increase in SpO2 in premature infants in lateral decubitus, which maintained the newborns in a position of flexion and the head in a favorable position for the pulmonary mechanism, exerting a direct influence on SpO221.
Two other studies investigated weight gain as the outcome. Comparing the hammock and nest methods, Keller et al.3 found no significant difference in weight gain but explained this lack of difference by the short intervention time, as the hammock method promotes relaxation and less energy expenditure. The other study compared the hammock and kangaroo methods and also found no statistically significant difference in weight gain or stay in the NICU11.
One of the limitations of the present systematic review was the small number of studies on the hammock method for preterm newborns. Greater information is needed on measures and results regarding motor improvements in these patients. Future studies should perform more detailed motor assessments to make the practice of this type of intervention viable for healthcare providers who seek to improve the quality of life of premature infants and enhance neuroprotective care in the NICU.
Quality of evidence
The quality of the evidence was appraised using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach, which is used to classify the body of evidence on the outcome level rather than the study level. To determine the strength of the recommendation, GRADE considers key factors, such as the risk of bias, inconsistency, indirectness, publication bias, and other distortions. The classification of quality has four levels of certainty in evidence: very low, low, moderate, and high. Interventions with a high level of certainty are strongly recommended. In the present systematic review and meta-analysis, a moderate level of certainty in the evidence was found for two outcomes: behavioral state (NBAS) and pain (NFCS) (Table 4).
Conclusions
The hammock method proved to be viable and promising for the reduction in pain/stress as well as the improvement in the behavioral state of preterm newborns. In contrast, no significant differences in heart rate or oxygen saturation were found in comparison to other intervention methods. Longitudinal studies are needed to confirm the neuroprotective importance of the hammock method as well as its effects on motor development in preterm newborns.
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Received 03.02.2021
Revised 19.02.2021
Accepted 24.02.2021

/76.jpg)
/79.jpg)
/78.jpg)
/80_2.jpg)
/80.jpg)
/81.jpg)