Журнал «Медицина неотложных состояний» Том 17, №8, 2021
Вернуться к номеру
Физиология обмена магния и применение магнезии в интенсивной терапии (литературный обзор с результатами собственных наблюдений, часть 3)
Авторы: Курсов С.В., Никонов В.В., Белецкий А.В., Киношенко Е.И., Скороплет С.Н.
Харьковская медицинская академия последипломного образования, г. Харьков, Украина
КНП «Харьковская клиническая больница скорой и неотложной помощи им. проф. А.И. Мещанинова» Харьковского городского совета, г. Харьков, Украина
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
Ми надали в цьому огляді результати експериментальних і клінічних досліджень, які найбільш переконливо демонструють місце порушень обміну магнію в розвитку пошкоджень міокарда, фатальних аритмій і артеріальної гіпертензії. Ми також висвітлили питання діагностики прихованого дефіциту магнію в організмі і роль дефіциту магнію в патогенезі кардіоміопатії, застійної серцевої недостатності і пролапсу мітрального клапана. Пероральні добавки Mg сприяють зниженню середнього артеріального тиску, периферичного опору судин і частоти ізольованих і залпових шлуночкових екстрасистол і нападів нестійкої шлуночкової тахіаритмії. Вчені виявили, що в багатьох пацієнтів із сильно вираженим пролапсом мітрального клапана рівень Mg в сироватці крові був низьким і прийом добавок з Mg призводить до поліпшення стану пацієнтів. Контроль статусу магнієвого обміну в організмі не тільки необхідний в умовах інтенсивної терапії та стаціонару в цілому, але також актуальний в амбулаторній практиці. Регулярний прийом препаратів Mg або харчових добавок, що містять в основному Mg, може істотно поліпшити результати лікування численних захворювань і запобігти розвитку небезпечних для організму ускладнень. При цьому собівартість магнезіальної терапії є досить низькою.
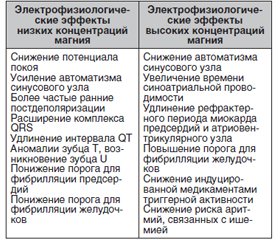
Мы представили в этом обзоре результаты экспериментальных и клинических исследований, которые наиболее убедительно демонстрируют место нарушений обмена магния (Mg) в развитии повреждений миокарда, фатальных аритмий и артериальной гипертензии. Мы также осветили вопросы диагностики скрытого дефицита магния в организме и роль дефицита магния в патогенезе кардиомиопатии, застойной сердечной недостаточности и пролапса митрального клапана. Пероральные добавки Mg способствуют снижению среднего артериального давления, периферического сопротивления сосудов и частоты изолированных и залповых желудочковых экстрасистол и приступов неустойчивой желудочковой тахиаритмии. Ученые обнаружили, что у многих пациентов с сильно выраженным пролапсом митрального клапана уровень Mg в сыворотке крови был низким и прием добавок с Mg приводил к улучшению состояния пациентов. Контроль статуса магниевого обмена в организме не только необходим в условиях интенсивной терапии и стационара в целом, но также актуален в амбулаторной практике. Регулярный прием препаратов Mg или пищевых добавок, содержащих Mg, может существенно улучшить результаты лечения множества заболеваний и предотвратить развитие опасных для организма осложнений. При этом себестоимость магнезиальной терапии является достаточно низкой.
In this review, we presented the results of experimental and clinical studies that most convincingly demonstrate the role of magnesium metabolism disorders in the development of myocardial damage, fatal arrhythmias, and arterial hypertension. We also highlighted the diagnosis of latent magnesium deficiency in the body and the role of magnesium deficiency in the pathogenesis of cardiomyopathy, congestive heart failure, and mitral valve prolapse. Oral Mg supplementation helps to reduce mean arterial pressure, peripheral vascular resistance, and the frequency of isolated and burst ventricular extrasystoles and attacks of unstable ventricular tachyarrhythmia. The researchers found that many patients with severe mitral valve prolapse had low serum Mg levels, and Mg supplementation was associated with improved patient outcomes. Monitoring the status of magnesium metabolism in the body is ne-cessary not only in intensive care and in the hospital as a whole but is also relevant in outpatient practice. The cost of magnesia therapy is quite low, but at the same time, regular intake of magnesium preparations or dietary supplements, containing mainly magnesium, can significantly improve the results of treatment of many diseases and prevent the development of complications that are dangerous for the body.
магній; дефіцит магнію; магнезіальна терапія; серцеві аритмії; ішемія і некроз міокарда; артеріальна гіпертензія; кардіоміопатія; застійна серцева недостатність; пролапс мітрального клапана, калій; натрій; кальцій
магний; дефицит магния; магнезиальная терапия; сердечные аритмии; ишемия и некроз миокарда; артериальная гипертензия; кардиомиопатия; застойная сердечная недостаточность; пролапс митрального клапана; калий; натрий; кальций
magnesium; magnesium deficiency; magnesium therapy; cardiac arrhythmias; myocardial ischemia and necrosis; arterial hypertension; cardiomyopathy; congestive heart failure; mitral valve prolapse; potassium; sodium; calcium
Введение
Материалы и методы
Результаты
/41.jpg)
/46.jpg)
Выводы
- Zwillinger L. On Magnesium's Effects on the Heart. Klin. Wochenschr. 1935. 14. 1429-33.
- Rothberger C.J., Zwillinger L. Über die Wirkung von Magnesium auf die Strophantin-and Barium-Tachykardie. Arch. Exp. Pathol. Pharmakol. 1936. 181. 301-16.
- Zwillinger L. Magnesium Sulfate in Paroxysmal Tachycardia. JAMA. 1939. 112(13). 1281. DOI: 10.1001/jama.1939.02800130065025.
- Lebr D. Magnesium and Cardiac Necrosis [Internet] Magnesium-Bulletin l a/1981 [New York Medical College, Westchester County Medical Center, Valhalla, New York] [cited 10 Aug 2021] 1981. P. 178-91. Available from: http://www.magnesium-ges.de/jdownloads/Literatur/Lehr %20D./lehr_1981_magnesium_and_cardiac_necrosis_449.pdf
- Antiarrhythmic Drugs. Mechanisms of Antiarrhythmic and Proarrhythmic Actions. Editors: G. Breithardt, M. Borggrefe, J.A. Camm, M. Shenasa. Berlin; Heidelberg: Springer-Verlag, 1995. 410 p. Available from: https: https://link.springer.com/book/10.1007/978-3-642-85624-2#toc
- Fleckenstein A. Specific Pharmacology of Calcium in Myocardium, Cardiac Pacemakers, and Vascular Smooth Muscle. Annu Rev. Pharmacal. & Toxicol. 1977. 17. 149-66. Available from: https://www.annualreviews.org/doi/abs/10.1146/annurev.pa.17.040177.001053
- Fleckenstein A. Metabolic Factors in the Development of Myocardial Necrosis and Microinfarcts. Triangle. 1975. 14(1). 27-36. Available from: https://pubmed.ncbi.nlm.nih.gov/1162727/
- Blaiklock R.G., Lukacsco A.B., Hirsh E., Lebr D. About the Mechanism of Epinephrine Induced Myocardial Necrosis. Pharmacologist. 1980. 22. 270.
- Brandt G., Dὂrfelt H.J. Postmortale Magnesiumkonzentrationen im Herz und Skelettmuskel. Leber, Mark und Rinde des Gehirns bei verschiedenen Grundleiden des Menschen: Krankenhausarzt. 1978. 51. 418-21.
- Levin R.M., Haugaard N., Hess M.E. Opposing Actions of Calcium and Magnesium Ions on the Metabolic Effects of Epinephrine in Rat Heart. Biochem. Pharm. 1976. Sep. 01. 25(17). 1963-9. DOI: 10.1016/0006-2952(76)90051-4
- Stühlinger H.G. Magnesium in Cardiovascular Disease. Journal of Clinical and Basic Cardiology. 2002. 5(1). 55-9. Available from: https://www.kup.at/kup/pdf/1047.pdf
- Stark G., Stark U., Tritthart H.A. Modulation of Cardiac Impulse Generation and Conduction by Nifedipine and Verapamil Analyzed by a Refined Surface ECG Technique in Langendorff Perfused Guinea Pig Hearts. Basic. Res. Cardiol. 1988. Mar-Apr. 83(2). 202-12. DOI: 10.1007/BF01907274
- Kulick D.L., Hong R., Ryzen E., Rude R.K., Rubin J.N., Elkayam U. et al. Electrophysiologic Effects of Intravenous Magnesium in Patients with Normal Conduction Systems and no Clinical Evidence of Significant Cardiac Disease. Am. Heart J. 1988. Feb. 115(2). 367-73. DOI: 10.1016/0002-8703(88)90483-8
- DiCarlo L.A. Jr, Morady F., de Buitleir M., Krol R.B., Schurig L., Annesley T.M. Effects of Magnesium Sulfate on Cardiac Conduction and Refractoriness in Humans. J. Am. Coll. Cardiol. 1986. Jun. 7(6). 1356-62. DOI: 10.1016/s0735-1097(86)80157-7
- Cohagan B., Brandis D. Torsade de Pointes [Internet] StatPearls [Last Update: August 11, 2021] Available from: https://www.ncbi.nlm.nih.gov/books/NBK459388/
- Rehman R., Hai O. Digitalis Toxicity [Internet] StatPearls [Last Update: July 17, 2021] Available from: https://www.ncbi.nlm.nih.gov/books/NBK459165/
- Custer A.M., Yelamanchili V.S., Lappin S.L. Multifocal Atrial Tachycardia [Internet] StatPearls [Last Update: July 22, 2021] Available from: https://www.ncbi.nlm.nih.gov/books/NBK459152/
- Lorentz M.N., Vianna B.S.B. Cardiac Dysrhythmias and Anesthesia. Rev. Bras. Anestesiol. 2011. Dec. 61(6). 798-813. Avai-lable from: https://www.scielo.br/j/rba/a/9WXDXZpNRdnNYbxjFs4Phsz/?format = pdf&lang = en
- Manrique A.M., Arroyo M., El Khoudary S.R., Colvin E., Lichtenstein S., Chrysostomou C. et al. Magnesium Supplementation during Cardiopulmonary Bypass to Prevent Junctional Ectopic Tachycardia after Pediatric Cardiac Surgery: A Randomized Controlled Study. Journal of Thoracic and Cardiovascular Surgery. 2010. Jan. 139(1). 162-9. e2. Available from: https://www.sciencedirect.com/science/article/pii/S0022522309010216
- Shiga T., Wajima Z. Magnesium Prophylaxis for Arrhythmias after Cardiac Surgery: A Meta-analysis of Randomized Controlled Trials. American Journal of Medicine. 2004. Sep. 01. 117. 325-33. Available from: https://ssl.rima.org/web/medline_pdf/AmJMed_ %20325.pdf
- Lim A.K.H., Azraai M., Pham J.H., Looi W.F., Wirth D., Ng A.S.L. et al. Severe Tachycardia Associated with Psychotropic Medications in Psychiatric Inpatients: A Study of Hospital Medical Emergency Team Activation. Journal of Clinical Medicine. 2021. Apr. 06. 10. 1534-45. Available from: https://doi.org/10.3390/jcm10071534
- Stoner S.C. Management of Serious Cardiac Adverse Effects of Antipsychotic Medications. Ment. Health Clin. 2017. Nov. 7(6). 246-54. DOI: 10.9740/mhc.2017.11.246
- Emamhadi M., Mostafazadeh B., Hassanijirdehi M. Tricyclic Antidepressant Poisoning Treated by Magnesium Sulfate: a Randomized, Clinical Trial. Drug. Chem. Toxicol. 2012. Jul. 35(3). 300-3. DOI: 10.3109/01480545.2011.614249
- Соловьян А.Н., Михалева Т.В., Михалев К.А. Классификация и механизмы действия антиаритмических препаратов. Ліки України. 2015. (4). 12-20. Available from: https://www.health-medix.com/articles/liki_ukr/2015-06-24/lec_1.pdf
- Sleeswijk M.E., Tulleken J.E., Van Noord T., Meertens J.H.J.M., Ligtenberg J.J.M., Zijlstra J.G. Efficacy of Magnesium-Amiodarone Step-Up Scheme in Critically Ill Patients with New-Onset Atrial Fibrillation: A Prospective Observational Study. Journal of Intensive Care Medicine. 2008. Jan. 23(1). 61-6. Available from: https://www.researchgate.net/publication/5531064
- Baker W.L. Treating Arrhythmias with Adjunctive Magnesium: Identifying Future Research Directions. European Heart Journal — Cardiovascular Pharmacotherapy. 2017. Apr. 3(2). 108-17. Available from: https://academic.oup.com/ehjcvp/article/3/2/108/2669829
- Allegra J., Lavery R., Cody R., Birnbaum G., Brennan J., Hartman J. et al. Magnesium Sulfate in the Treatment of Refractory Ventricular Fibrillation in the Prehospital Setting. Resuscitation. 2001. Jun. 49(3). 245-9. DOI: 10.1016/s0300-9572(00)00375-0
- Ho K.M. Intravenous Magnesium for Cardiac Arrhythmias: Jack of all Trades. Magnesium Research. 2008. Mar. 21(1). 65-8. Available from: https://www.jle.com/en/revues/mrh/e-docs/intravenous_magnesium_for_cardiac_arrhythmias_jack_of_all_trades_277381/article.phtml
- Neiger J.S., Gupta A., Halleran S.M., Trohman R.G. Magnesium Sensitive, Adenosine Resistant, Repetitive Monomorphic Ventricular Tachycardia. Pacing. Clin. Electrophysiol. 2009. Dec. 32(12). e28-30. DOI: 10.1111/j.1540-8159.2009.02527.x
- Trappe H.J. Treating Critical Supraventricular and Ventricular Arrhythmias. Journal Emerg. Trauma Shock. 2010. Apr-Jun. 3(2). 143-52. DOI: 10.4103/0974-2700.62114
- Smetana R., Sthlinger G., Kiss K., Glogar D.H. Intravenous Magnesium Sulphate in Acute Myocardial Infarction — Is the answer “MAGIC”? Magnesium Research. 2003. Mar. 16(1). 63-9. Available from: https://www.jle.com/en/revues/mrh/e-docs/intravenous_magnesium_sulphate_in_acute_myocardial_infarction_is_the_answer_magic__260690/article.phtml
- Rasmussen H.S., Larsen O.G., Meier K., Larsen J. Hemodynamic Effects of Intravenously Administered Magnesium on Patients with Ischemic Heart Disease. Clin. Cardiol. 1988. Dec. 11(12). 824-8. DOI: 10.1002/clc.4960111205
- Teo K.K., Yusuf S., Held P.H., Peto R. Effects of Intravenous Magnesium in Suspected Acute Myocardial Infarction: Overview of Randomised Trials. BMJ. 1991. Dec. 14. 03(6816). 1499-1503. DOI: 10.1136/bmj.303.6816.1499
- Woods K.L., Fletcheer S., Foffe C., Haider Y. Intravenous Magnesium Sulphate in Suspected Acute Myocardial Infarction. Results of the Second Leicester Intravenous Magnesium Intervention Trial (LIMIT-2). Lancet. 1992. Jun. 27. 339(8809). 1553-8. DOI: 10.1016/0140-6736(92)91828-v
- Семиголовский Н.Ю. Калий, магний и летальность кардиологических больных. Трудный пациент. 2014. (7). 32-6. Available from: https://t-pacient.ru/wp-content/uploads/2014/09/TP-7-2014.pdf
- Liao F., Folsom A.R., Brancati F.L. Is Low Magnesium Concentration a Risk Factor for Coronary Heart Disease? The Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 1998. Sep. 136(3). 480-90. DOI: 10.1016/s0002-8703(98)70224-8
- Вдовиченко В.П., Гончарук В.В., Коршак Т.А., Бронская Г.М. Препараты калия/магния: рациональные основы применения в клинике. Медицинские новости. 2016. (11). 8-10. Available from: https://cyberleninka.ru/article/n/preparaty-kaliya-magniya-ratsionalnye-osnovy-primeneniya-v-klinike
- Shechter M., Sharir M., Labrador M.J., Forrester J., Silver B., Bairey Merz C.N. Oral Magnesium Therapy Improves Endothelial Function in Patients with Coronary Artery Disease. Circulation. 2000. Nov 7. 102(19). 2353-8. DOI: 10.1161/01.cir.102.19.2353
- Satake K., Lee J.-D., Shimizu H., Uzui H., Mitsuke Y., Yue H. et al. Effects of Magnesium on Prostacyclin Synthesis and Intracellular Free Calcium Concentration in Vascular Cells. Magnesium Research. 2004. Mar. 17(1). 20-7. Available from: https://www.jle.com/en/revues/mrh/e-docs/effects_of_magnesium_on_prostacyclin_synthesis_and_intracellular_free_calcium_concentration_in_vascular_cells__262005/article.phtml
- Shechter M. Magnesium and Cardiovascular System. Magnesium Research. 2010. Jun. 23(2). 60-72. Available from: https://www.jle.com/en/revues/mrh/e-docs/magnesium_and_cardiovascular_system_285054/article.phtml
- Василевский И.В. Новая форма адъювантной терапии в клинической медицине. Международные обзоры: клиническая практика и здоровье. 2018. (1). 70-8. Available from: https://mail.google.com/mail/u/0/?tab = rm&ogbl#inbox/FMfcgzGkZstnWRhQktgpFcLsvmwXNrpj?projector = 1&messagePartId = 0.2
- DiNicolantonio J.J., Liu J., O’Keefe J.H. Magnesium for the Prevention and Treatment of Cardiovascular Disease [Internet] BMJ: Open Heart. 2018. 5. e000775. DOI: 10.1136/openhrt-2018-000775
- Guo H., Cheng J., Lee J.D., Ueda T., Shan J., Wang J. Relationship between the Degree of Intracellular Magnesium Deficiency and the Frequency of Chest Pain in Women with Variant Angina. Herz. 2004. May. 29(3). 299-303. DOI: 10.1007/s00059-003-2471-2
- Teragawa H., Kato M., Yamagata T., Matsuura H., Kajiyama G. The Preventive Effect of Magnesium on Coronary Spasm in Patients with Vasospastic Angina. Chest. 2000. Dec. 118(6). 1690-5. DOI: 10.1378/chest.118.6.1690
- Li J., Zhang Q., Zhang M., Egger M. Intravenous Magnesium for Acute Myocardial Infarction (Review) [Internet] Cochrane Library: Cochrane Database of Systematic Reviews. 2007. Is. 2. Article: CD002755. DOI: 10.1002/14651858.CD002755.pub2
- Salaminia S., Sayehmiri F., Angha P., Sayehmiri K., Mote-dayen M. Evaluating the Effect of Magnesium Supplementation and Cardiac Arrhythmias after Acute Coronary Syndrome: a Systematic Review and Meta-analysis. BMC Cardiovascular Disorders. 2018. Jun 28. 18. Article 129. Available from: https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-018-0857-6
- Szapary L.B., Szakacs Z., Farkas N., Schonfeld K., Babocsay D., Gajer M. et al. The Effect of Magnesium on Reperfusion Arrhythmias in STEMI Patients, Treated with PPCI. A Systematic Review with a Meta-Analysis and Trial Sequential Analysis. Frontiers Cardiovasc Med. 2021. Jan. 11. 7. 608193. DOI: 10.3389/fcvm.2020.608193
- Jee H.L., Miller E.R., Guallar E., Singh V.K., Appel L.J., Klag M.J. The Effect of Magnesium Supplementation on Blood Pressure: a Meta-analysis of Randomized Clinical Trials. Am. J. Hypertens. 2002. Aug. 15(8). 691-6. DOI: 10.1016/s0895-7061(02)02964-3.
- Touyz R.M. Role of Magnesium in the Pathogenesis of Hypertension. Mol. Aspects Med. 2003. Feb-Jun. 24(1–3). 107-36. DOI: 10.1016/s0098-2997(02)00094-8
- Skrzek A., Stolarz-Skrzypek K., Kocek M., Czarnecka D. Magnesium Supplementation in Patients with Hypertension. Przegl. Lek. 2016. 73(6). 368-72. Available from: https://pubmed.ncbi.nlm.nih.gov/29668203/
- Zhang X., Li Y., Del Gobbo L.C., Rosanoff A., Wang J., Zhang W. et al. Effects of Magnesium Supplementation on Blood Pressure. A Meta-Analysis of Randomized Double-Blind Placebo-Controlled Trials. Hypertension. 2016. Jul. 11. 68. 324-33. Available from: https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.116.07664
- Kawano Y., Matsuoka H., Takishita S., Omae T. Effects of Magnesium Supplementation in Hypertensive Patients Assessment by Office, Home, and Ambulatory Blood Pressures. Hypertension. 1998. Aug. 32(2). 260-5. Available from: https://www.ahajournals.org/doi/10.1161/01.HYP.32.2.260
- Kass L., Weekes J., Carpenter L. Effect of Magnesium Supplementation on Blood Pressure: a Meta-Analysis. European Journal of Clinical Nutrition. 2012. Feb. 08. 66. 411-8. Available from: https://www.nature.com/articles/ejcn20124
- Rosanoff A., Plesset M.R. Oral Magnesium Supplements Decrease High Blood Pressure (SBP > 155 mm Hg) in Hypertensive Subjects on Anti-Hypertensive Medications: a Targeted Meta-Analysis. Magnesium Research. 2013. Jul-Sep. 26(3). 93-9. DOI: 10.1684/mrh.2013.0343
- Han H., Fang X., Wei X., Liu Y., Jin Z., Chen Q. et al. Dose-Response Relationship between Dietary Magnesium Intake, Serum Magnesium Concentration and Risk of Hypertension: a Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutr. J. 2017. May 05. 16(1). 26. DOI: 10.1186/s12937-017-0247-4
- Yanti M.D., Suromo L.B. The Correlation between Serum Magnesium Level and Blood Pressure in Patient with Chronic Kidney Disease. Intisari Sains Medis. 2019. 10(1). 238-41. DOI: 10.1556/ism.v10i1.359
- Rosanoff A., Costello R.B., Johnson G.H. Effectively Prescribing Oral Magnesium Therapy for Hypertension: A Categorized Systematic Review of 49 Clinical Trials. Nutrients. 2021. 13(1). 195-209. Available from: https://www.mdpi.com/2072-6643/13/1/195
- DiNicolantonio J.J., O’Keefe J.H, Wilson W. Subclinical Magnesium Deficiency: a Principal Driver of Cardiovascular Di-sease and a Public Health Crisis [Internet] Open Heart. 2018. 5(1). 000668. DOI: 10.1136/ openhrt-2017-000668
- Jahnen-Dechent W., Ketteler M. Magnesium Basics. Clin. Kidney J. 2012. Feb. 5(Suppl. 1). i3-i14. DOI: 10.1093/ndtplus/sfr163
- Cascella M., Vaqar S. Hypermagnesemia [Internet] StatPearls (Last Update: July 17, 2021) Available from: https://www.ncbi.nlm.nih.gov/books/NBK549811/
- Gullestad L., Dolva L.O., Waage A., Falch D., Fagerthun H., Kjekshus J. Magnesium Deficiency Diagnosed by an Intravenous Loading Test. Scand. J. Clin. Lab. Invest. 1992. Jun. 52(4). 245-53. DOI: 10.3109/00365519209088355
- Gullestad L., Midtvedt K., Dolva L.O., Norseth J., Kjekshus J. The Magnesium Loading Test: Reference Values in Healthy Subjects. Scand. J. Clin. Lab. Invest. 1994. Feb. 54(1). 23-31. DOI: 10.3109/00365519409086506
- Gullestad L., Nes M., Ronneberg R., Midtvedt K., Falch D., Kjekshus J. Magnesium Status in Healthy Free-Living Elderly Norwegians. J. Am. Coll. Nutr. 1994. Feb. 13(1). 45-50. DOI: 10.1080/07315724.1994.10718370
- Uğurlu V., Binay Ç., Şimşek E., Bal C. Cellular Trace Element Changes in Type 1 Diabetes Patients. J. Clin. Res. Pediatr. Endocrinol. 2016. 8(2). 180-6. Available from: http://cms.galenos.com.tr/Uploads/Article_1529/JCRPE-8-180.pdf
- Simşek E., Karabay M., Kocabay K. Assessment of Magnesium Status in Newly Diagnosed Diabetic Children: Measurement of Erythrocyte Magnesium Level and Magnesium Tolerance Tes-ting. Turk. J. Pediatr. 2005. Apr-Jun. 47(2). 132-7. Available from: https://pubmed.ncbi.nlm.nih.gov/16052852/
- Houston M. The Role of Magnesium in Hypertension and Cardiovascular Disease. Journal of Clinical Hypertension. 2011. Nov. 13(11). 843-7. Available from: https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1751-7176.2011.00538.x
- Yamori Y., Taguchi T., Mori H., Mori M. Low Cardiovascular Risks in the Middle Aged Males and Females Excreting Greater 24-Hour Urinary Taurine and Magnesium in 41 WHO-CARDIAC Study Populations in the World. J. Biomed. Sci. 2010. Aug 24. 17(Suppl. 1). S21. DOI: 10.1186/1423-0127-17-S1-S21
- Preuss H.G. Diet, Genetics and Hypertension. J. Am. Coll. Nutr. 1997. Aug. 16(4). 296-305. DOI: 10.1080/07315724.1997.10718690
- Das U.N. Delta-6 Desaturase as the Target of the Bene-ficial Actions of Magnesium. Medical Science Monit. 2010. Aug. 16(8). LE11-2. Available from: https://pubmed.ncbi.nlm.nih.gov/20671618/
- Das U.N. Essential Fatty Acids: Biochemistry, Physiology and Pathology. Biotechnol. J. 2006. Apr. 1(4). 420-39. DOI: 10.1002/biot.200600012
- Resnick L. The Cellular Ionic Basis of Hypertension and Allied Clinical Conditions. Progress in Cardiovascular Diseases. 1999. Jul. 01. 42(1). 1-22. DOI: 10.1016/s0033-0620(99)70006-x
- Jia E.Z., Yang Z.J., Zhu T.B., Wang L.S., Chen B., Cao K.J. et al. Serum Sodium Concentration is Significantly Associated with the Angiographic Characteristics of Coronary Atherosclerosis. Acta Pharmacologica Sinica. 2007. Aug. 28 (8). 1136-42. DOI: 10.1111/j.1745-7254.2007.00597.x
- Wongdee K., Rodrat M., Teerapornpuntakit J., Krishnamra N., Charoenphandhu N. Factors Inhibiting Intestinal Calcium Absorption: Hormones and Luminal Factors that Prevent Excessive Calcium Uptake. Journal of Physiological Sciences. 2019. 69. 683-96. Available from: https://jps.biomedcentral.com/articles/10.1007/s12576-019-00688-3
- Liu M., Liu H., Feng F., Xie A., Kang G.J., Zhao Y. et al. Magnesium Deficiency Causes a Reversible, Metabolic, Diastolic Cardiomyopathy. Journal of the American Heart Association. 2021. Jun. 05. 10(12). e020205. Available from: https://www.ahajournals.org/doi/full/10.1161/JAHA.120.020205
- Ahmad A., Bloom S. Sodium Pump and Calcium Channel Modulation of Mg-Deficiency Cardiomyopathy. Am. J. Cardiovasc. Pathol. 1989. 2(4). 277-83. Available from: https://pubmed.ncbi.nlm.nih.gov/2551352/
- Herbaczynska-Cedro K., Gajkowska B. Effect of Magnesium on Myocardial Damage Induced by Epinephrine. Ultrastructural and Cytochemical Study. Cardioscience. 1992. Sep. 3(3). 197-203. Avai-lable from: https://pubmed.ncbi.nlm.nih.gov/1420956/
- Valiathan S.M., Kartha C.C. Endomyocardial fibrosis — the possible connexion with myocardial levels of magnesium and cerium. Int. J. Cardiol. 1990. Jul. 28(1). 1-5. DOI: 10.1016/0167-5273(90)90002-m.
- Douban S., Brodsky M.A., Whang D.D., Whang R. Significance of Magnesium in Congestive Heart Failure. Am. Heart J. 1996. Sep. 132(3). 664-71. DOI: 10.1016/s0002-8703(96)90253-7
- Nishihara T., Yamamoto E., Sueta D., Fujisue K., Usuku H., Oike F. et al. Clinical Significance of Serum Magnesium Levels in Patients with Heart Failure with Preserved Ejection Fraction. Medicine. 2019. Sep. 98(38). e17069. DOI: 10.1097/MD.0000000000017069
- Gaulden J.K., Appel S.J., Kilcawley V. Micronutrients in Congestive Heart Failure: An Integrative Review. Int. Arch. Nurs. Health Care. 2018. 4(2). 095. Available from: doi.org/10.23937/2469-5823/1510095
- Bashir Y., Sneddon J.F., Staunton H.A., Haywood G.A., Simpson I.A., McKenna W.J. et al. Effects of Long-Term Oral Magnesium Chloride Replacement in Congestive Heart Failure Secondary to Coronary Artery Disease. Am. J. Cardiol. 1993. Nov. 15. 72(15). 1156-62. DOI: 10.1016/0002-9149(93)90986-m
- Gottlieb S.S., Baruch L., Kukin M.L., Bernstein J.L., Fi-sher M.L., Packer M. Prognostic Importance of the Serum Magnesium Concentration in Patients with Congestive Heart Failure. J. Am. Coll. Cardiol. 1990. Oct. 16(4). 827-31. DOI: 10.1016/s0735-1097(10)80329-8
- University of Minnesota Medical School. Study Suggests how to Treat Diastolic Heart Failure. Research Shows Magnesium Improves a Form of Heart Failure Previously without Treatment [Internet] Science Daily (January 10, 2019. cited 19 Sep 2021) Available from: https://www.sciencedaily.com/releases/2019/01/190110141730.htm
- Song E.K., Kang S.M. Micronutrient Deficiency Independently Predicts Adverse Health Outcomes in Patients with Heart Fai-lure. J. Cardiovasc. Nurs. 2017. Jan-Feb. 2017. 32(1). 47-53. DOI: 10.1097/JCN.0000000000000304
- Lichodziejewska B., Kłoś J., Rezler J., Grudzka K., Dłuzniewska M., Budaj A. et al. Clinical Symptoms of Mitral Valve Prolapse Are Related to Hypomagnesemia and Attenuated by Magnesium Supplementation. Am. J. Cardiol. 1997. Mar. 15. 79(6). 768-72. DOI: 10.1016/s0002-9149(96)00865-x
- Kitliński M., Stepniewski M., Nessler J., Konduracka E., Solarska K., Piwowarska W. et al. Is Magnesium Deficit in Lymphocytes a Part of the Mitral Valve Prolapse Syndrome? Magnesium Research. 2004. Mar. 17(1). 39-45. Available from: https://pubmed.ncbi.nlm.nih.gov/15083568/
- Bobkowski W., Nowak A., Durlach J. The Importance of Magnesium Status in the Pathophysiology of Mitral Valve Prolapse. Magnesium Research. 2005. Mar. 18(1). 35-52. Available from: https://www.jle.com/en/revues/mrh/e-docs/the_importance_of_magnesium_status_in_the_pathophysiology_of_mitral_valve_prolapse_265367/article.phtml