Журнал «Медицина неотложных состояний» Том 18, №1, 2022
Вернуться к номеру
Синдром сонного апное у практиці амбулаторної анестезії (літературний огляд)
Авторы: Кріштафор Д.А., Клигуненко О.М., Станін Д.М.
Дніпровський державний медичний університет, м. Дніпро, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
Синдром обструктивного апное сну є досить частим станом, на який іноді не звертають уваги. Основним його проявом є припинення самостійного дихання уві сні з частотою понад 5 раз на годину з пробудженнями, порушенням сну і, як наслідок, денною сонливістю. Найбільш часто синдром обструктивного апное сну поєднується з ожирінням. Визнано, що існує зв’язок між цим захворюванням і гіпертонією, ішемічною хворобою серця, інсультами. Діагностика вимагає спеціальних методів дослідження, таких як полісомнографія. Існують досить прості опитувальники, що дозволяють запідозрити це захворювання (шкала Епворт, опитувальник STOP-Bang). В амбулаторній хірургії синдром обструктивного апное сну (в поєднанні з ожирінням) представляє небезпеку за рахунок складних дихальних шляхів, ризику апное при виході з наркозу, раптової смерті у післяопераційному періоді. В даному огляді наведені методи корекції цього захворювання, особливості передопераційної оцінки хворих, інтраопераційного ведення, особливості пробудження в постнаркозному періоді.
Obstructive sleep apnea is a common and often overlooked condition. Its main manifestation is the pause of spontaneous breathing during sleep with a frequency of more than five times per hour with awakenings, sleep disturbances and, as a result, daytime sleepiness. Obstructive sleep apnea is most commonly associated with obesity. It is recognized that there is a link between this disease and hypertension, coronary heart disease, and strokes. Diagnosis requires special research methods such as polysomnography. There are fairly simple questionnaires that allow suspecting this condition (Epworth scale, STOPBang questionnaire). In outpatient surgery, obstructive sleep apnea syndrome (in combination with obesity) is dangerous due to difficult airways, the risk of apnea upon recovery from anesthesia, sudden death in the postoperative period. This review presents methods of correction of this condition, features of the preoperative assessment of patients, intraoperative management, and features of awakening in the post-anesthetic period.
синдром обструктивного апное сну; сонне апное; амбулаторна хірургія; огляд
obstructive sleep apnea; sleep apnea; outpatient surgery; review
Клінічні особливості
Діагностика
/29.jpg)
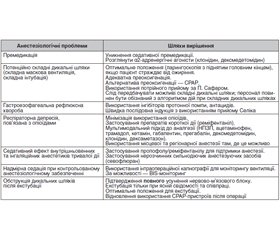
Періопераційне ведення пацієнтів із СОАС в амбулаторній хірургії
Висновки
- Raeder J. Clinical Ambulatory Anesthesia. Cambridge: Cambridge University Press, 2010. 185 p.
- Shetty A., Raveendra U.S. Anesthesia for day care surgery. Journal of Health and Allied Sciences NU. 2015. Vol. 05(02). P. 97-103. doi: 10.1055/s-0040-1703901.
- Lee J.H. Anesthesia for ambulatory surgery. Korean J. Anesthesiol. 2017. Vol. 70(4). P. 398-406. doi: 10.4097/kjae.2017.70.4.398.
- Royal College of Anaesthetists. Guidance on the provision of anaesthetic care in the non-theatre environment. London, UK, 2019. 28 p.
- Royal College of Anaesthetists. Guidelines for the Provision of Anaesthesia Services for Day Surgery. London, UK, 2020. 28 p.
- American Society of Anesthesiologists. Guidelines for office based anesthesia. Committee of Origin: Ambulatory Surgical Care. 2019. URL: https://www.asahq.org/standards-and-guidelines/guidelines-for-office-based-anesthesia.
- Maciejewski D. Guidelines for system and anaesthesia organization in short stay surgery (ambulatory anaesthesia, anaesthesia in day case surgery). Anaesthesiology Intensive Therapy. 2013. Vol. 45. № 4. P. 190-199. doi: 10.5603/AIT.2013.0038.
- Bailey C.R., Ahuja M., Bartholomew K. et al. Guidelines for day-case surgery 2019. Anaesthesia. 2019. Vol. 74. P. 778-792. doi: 10.1111/anae.14639.
- Mannarino M.R., Di Filippo F., Pirro M. Obstructive sleep apnea syndrome. European Journal of Internal Medicine. 2012. Vol. 23. P. 586-593. doi: 10.1016/j.ejim.2012.05.013.
- Bixler E.O., Vgontzas A.N., Ten Have T. et al. Effects of age on sleep apnoea in men: prevalence and severity. Am. J. Respir. Crit. Care Med. 1998. Vol. 157. P. 144-148. doi: 10.1164/ajrccm.157.1.9706079.
- Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998. Vol. 102. P. 616-620. doi: 10.1542/peds.102.3.616.
- Redline S., Tishler P.V., Hans M.G. et al. Racial differences in sleep-disordered breathing in African-Americans. Am. J. Respir. Crit. Care Med. 1997. Vol. 155. P. 186-192. doi: 10.1164/ajrccm.155.1.9001310.
- Tuomilehto H.P., Seppa J., Partinen M. et al. Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnoea. Am. J. Respir. Crit. Care Med. 2009. Vol. 179. P. 320-327. doi: 10.1164/rccm.200805-669OC.
- Carskadon M.A., Dement W.C., Mitler M.M. et al. Guidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepiness. Sleep. 1986. Vol. 9. P. 519-524. doi: 10.1093/sleep/9.4.519.
- Gonzalez-Aquines A., Martinez-Roque D., Baltazar Trevino-Herrera A. et al. Obstructive sleep apnea syndrome and its relationship with ischaemic stroke. Rev. Neurol. 2019. Vol. 69(6). P. 255-260. doi: 10.33588/rn.6906.2019061.
- Krakow B., Melendrez D., Ferreira E. et al. Prevalence of insomnia symptoms in patients with sleep disordered breathing. Chest. 2001. Vol. 120. Р. 1923-1929. doi: 10.1378/chest.120.6.1923.
- Sangal R.B., Thomas L., Mitler M.M. Maintenance of wakefulness test and multiple sleep latency test. Measurement of different abilities in patients with sleep disorders. Chest. 1992. Vol. 101. P. 898-902. doi: 10.1378/chest.101.4.898.
- Johns M.W. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991. Vol. 14. P. 540. doi: 10.1093/sleep/14.6.540.
- Horstmann S., Hess C.W., Bassetti C. et al. Sleepiness-related accidents in sleep apnea patients. Sleep. 2000. Vol. 23. P. 383.
- Jordan A., McEvoy R.D. Gender differences in sleep apnea: epidemiology, clinical presentation and pathogenic mechanisms. Sleep Med. Rev. 2003. Vol. 7. P. 377-389. doi: 10.1053/smrv.2002.0260.
- Gold A.R., Dipalo F., Gold M.S., O’Hearn D. The symptoms and signs of upper airway resistance syndrome: a link to the functional somatic syndromes. Chest. 2003. Vol. 123. P. 87-95. doi: 10.1378/chest.123.1.87.
- Gold A.R., Dipalo F., Gold M.S., Broderick J. Inspiratory airflow dynamics during sleep in women with fibromyalgia. Sleep. 2004. Vol. 27. P. 459-466. doi: 10.1093/sleep/27.3.459.
- Bonsignore M.R., Saaresranta T., Riha R.L. Sex differences in obstructive sleep apnoea. Eur. Respir. Rev. 2019. Vol. 28(154). Article No.190030. doi: 10.1183/16000617.0030-2019.
- Fietze I., Laharnar N., Obst A. et al. Prevalence and association analysis of obstructive sleep apnea with gender and age differences — Results of SHIP-Trend. J. Sleep Res. 2019. Vol. 28(5). P. e12770. doi: 10.1111/jsr.12770.
- The Report of an American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999. Vol. 22. P. 667-689.
- Tuomilehto H.P., Seppa J., Partinen M. et al. Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnoea. Am. J. Respir. Crit. Care Med. 2009. Vol. 179. P. 320-327. doi: 10.1164/rccm.200805-669OC.
- Pepperell J., Ramdassingh-Dow S., Crosthwaite N., et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomized parallel trial. Lancet. 2002. Vol. 359. P. 204-210. doi: 10.1016/S0140-6736(02)07445-7.
- Jenkinson C., Davies R.J., Mullins R., Stradling J.R. Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomized prospective parallel trial. Lancet. 1999. Vol. 353. P. 2100-2105. doi: 10.1016/S0140-6736(98)10532-9.
- Hack M., Davies R.J., Mullins R. et al. Randomised prospective parallel trial of therapeutic versus subtherapeutic nasal continuous positive airway pressure on simulated steering performance In patients with obstructive sleep apnoea. Thorax. 2000. Vol. 55. P. 224-231. doi: 10.1136/thorax.55.3.224.
- Smith I., Lasserson T.J., Wright J. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst. Rev. 2006. Article No. CD003002. doi: 10.1002/14651858.CD003002.pub2.
- Ferguson K.A., Love L.L., Ryan C.F. Effect of mandibular and tongue protrusion on upper airway size during wakefulness. Am. J. Respir. Crit. Care Med. 1997. Vol. 155. Р. 1748-1754. doi: 10.1164/ajrccm.155.5.9154887.
- Redline S., Adams N., Strauss M.E. et al. Improvement of mild sleep-disordered breathing with CPAP compared with conservative therapy. Am. J. Respir. Crit. Care Med. 1998. Vol. 157. P. 858-865. doi: 10.1164/ajrccm.157.3.9709042.
- Gross J.B., Bachenberg K.L., Benumof J.L. et al. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology. 2006. Vol. 106. P. 1081-1093. doi: 10.1097/00000542-200605000-00026.
- Gross J.B., Apfelbaum J.L., Caplan R.A. et al. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology. 2014. Vol. 120. P. 268-286. doi: 10.1097/ALN.0000000000000053.
- Raveendran R., Chung F. Ambulatory anesthesia for patients with sleep apnea. Ambulatory Anesthesia. 2015. Vol. 2. P. 143-151. doi: 10.2147/AA.S63819.
- Joshi G.P., Ankichetty S.P., Gan T.J., Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth. Analg. 2012. Vol. 115. P. 1060-1068. doi: 10.1213/ANE.0b013e318269cfd7.
- Joshi G.P., Ahmad S., Riad W. et al. Selection of obese patients undergoing ambulatory surgery: a systematic review of the literature. Anesth. Analg. 2013. Vol. 117. P. 1082-1091. doi: 10.1213/ANE.0b013e3182a823f4.
- Joshi G.P., Ankichetty S.P., Gan T.J., Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth. Analg. 2012. Vol. 115. P. 1060-1068. doi: 10.1213/ANE.0b013e318269cfd7.
- Stierer T.L., Wright C., George A. et al. Risk assessment of obstructive sleep apnea in a population of patients undergoing ambulatory surgery. J. Clin. Sleep Med. 2010. Vol. 6. P. 467-472.
- Siyam M.A., Benhamou D. Difficult endotracheal intubation in patients with sleep apnea syndrome. Anesth. Analg. 2002. Vol. 95. P. 1098-1102. doi: 10.1097/00000539-200210000-00058.
- Gonzalez H., Minville V., Delanoue K. et al. The importance of increased neck circumference to intubation difficulties in obese patients. Anesth. Analg. 2008. Vol. 106. P. 1132-1136. doi: 10.1213/ane.0b013e3181679659.
- Reinius H., Jonsson L., Gustafsson S. et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology. 2009. Vol. 111. P. 979-987. doi: 10.1097/ALN.0b013e3181b87edb.
- Futier E., Constantin J.M., Pelosi P. et al. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology. 2011. Vol. 114. P. 1354-1363. doi: 10.1097/ALN.0b013e31821811ba.
- Aldenkortt M., Lysakowski C., Elia N. et al. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br. J. Anaesth. 2012. Vol. 109. P. 493-502. doi: 10.1093/bja/aes338.
- Grosse-Sundrup M., Henneman J.P., Sandberg W.S. et al. Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative respiratory complications: prospective propensity score matched cohort study. BMJ. 2012. Vol. 345. P. e6329. doi: 10.1136/bmj.e6329.
- Murphy G.S., Brull S.J. Residual neuromuscular block: lessons unlearned. Part I: definitions, incidence, and adverse physiologic effects of residual neuromuscular block. Anesth. Analg. 2010. Vol. 111. P. 120-128. doi: 10.1213/ANE.0b013e3181da832d.
- Popat M., Mitchell V., Dravid R. et al. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia. 2012. Vol. 67. P. 318-340. doi: 10.1111/j.1365-2044.2012.07075.x.
- Sundar E., Chang J., Smetana G.W. Perioperative screening for and management of patients with obstructive sleep apnea. J. Clin. Outcomes Manag. 2011. Vol. 18. P. 399-411.
- Marcus C.L., Brooks L.J., Draper K.A. et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012. Vol. 130. P. 576-584. doi: 10.1542/peds.2012-1671.
- Roland P.S., Rosenfeld R.M., Brooks L.J. et al. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol. Head Neck Surg. 2011. Vol. 145. P. S1-S15. doi: 10.1177/0194599811409837.
- Baugh R.F., Archer S.M., Mitchell R.B. et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol. Head Neck Surg. 2011. Vol. 144. P. S1-S30. doi: 10.1177/0194599810389949.
- Subramanyam R., Varughese A., Willging J.P., Sadhasivam S. Future of pediatric tonsillectomy and perioperative outcomes. Int. J. Pediatr. Otorhinolaryngol. 2013. Vol. 77. P. 194-199. doi: 10.1016/j.ijporl.2012.10.016.
- Seet E., Chung F. Management of sleep apnea in adults — functional algorithms for the perioperative period: Continuing Professional development. Can. J. Anaesth. 2010. Vol. 57. P. 849-864. doi: 10.1007/s12630-010-9344-y.
- Chung F., Liao P., Yegneswaran B. et al. Postoperative changes in sleep-disordered breathing and sleep architecture in patients with obstructive sleep apnea. Anesthesiology. 2014. Vol. 120. P. 287-298. doi: 10.1097/ALN.0000000000000040.

/30.jpg)
/31.jpg)