Introduction
Atrial fibrillation (AF) is currently the most common form of arrhythmias [1] and one of the most common causes of disabling cerebral thromboembolism and readmission to hospital. At the same time, the very specificity of the disease (clinical symptoms, consequences, features of therapy) determines its significant impact on the actual life situation, the patient’s emotional state and intellect [2].
AF, in addition to severe cerebral complications such as thromboembolic stroke, promotes hypoperfusion of vital organs due to fluctuations in cardiac output [3], and also combines with significant metabolic, neuroendocrine and other shifts [4]. All of these can also affect cognitive abilities.
The cognitive implications of AF in non-elderly patients may be subtle, but still present some difficulties in everyday life. For example, cognitive impairment reduces adherence to anticoagulant therapy, which, in turn, through a vicious circle mechanism, increases the likelihood of thromboembolic complications and further cognitive decline [5].
Large-scale scientific studies carried out in the last decade indicate that one of the promising directions for the prevention of cognitive disorders can be adequate antiarrhythmic therapy [6]. Of considerable interest is the effect on the cognitive functions of drugs prescribed to correct AF. Currently, for the treatment of cardiac arrhythmias both medical and surgical treatments are used. There are two main directions in the treatment of patients with AF: rhythm and heart rate control. Restoration of sinus rhythm allows not only to reduce cardiac symptoms and improve quality of life of a patient, but also to restore the myocardial contracti-lity, to prevent severe complications.
In the scientific literature, there are almost no works that study the dynamics of cognitive disorders in patients with AF as a result of successful pharmacological cardioversion.
Choosing the right treatment strategy for arrhythmias can slow the progression of cognitive deficits, which will improve not only the clinical status of patients, but also their prognosis. The above positions determined the relevance of the chosen direction of research and its purpose.
The purpose of our work was to evaluate the effect of successful pharmacological cardioversion (amiodarone) on the neurological symptoms and cognitive functions in patients with paroxysmal AF.
Materials and methods
One hundred and sixteen patients aged 30 to 75 years (mean of 62.2 ± 4.2 years) with cognitive disorders on the background of paroxysmal AF were examined. Tachysystolic form of AF at the time of hospitalization was detected in 82.7 % of cases. Short paroxysms (3–4 complexes) were recorded in 21 (18.1 %) people. In 38 (32.7 %) patients, pa-roxysmal AF was diagnosed for the first time, in 72 (62.1 %) cases, it was difficult to determine the age of arrhythmia detection. Mild cognitive disorders were diagnosed in 50 (52 %) cases, moderate — in 61 (38.1 %), and severe cognitive disorders — in 28 (9.9 %) patients.
Inclusion criteria without research assistance:
1. Age up to 75 years;
2. The patient’s ability to make productive contact with the doctor to assess the cognitive status;
3. Voluntary informed consent of the patient or, if necessary, the consent of the person caring for the patient;
4. Lack of regular antihypertensive and antiarrhythmic drug therapy for at least 12 weeks before inclusion in the study.
Criteria for excluding patients from the study:
1. Lack of voluntary informed consent of the patient;
2. Vascular dementia (Mini-Mental State Examination (MMSE) < 24, Frontal Assessment Battery (FAB) < 11, Mattis Dementia Rating Scale (DRS) < 115 points);
3. Other possible causes of CD, in addition to cerebrovascular disease: Parkinson’s disease and parkinsonism syndrome, Huntington’s disease, Wilson-Konovalov disease, normal pressure hydrocephalus, brain tumors (primary and metastatic), neuroinfections, epilepsy, demyelinating di-seases, Alzheimer’s disease, frontotemporal degeneration, dementia with Lewy bodies;
4. Brain injuries and their consequences, which are the only cause of cognitive deficit;
5. Acute disorders of cerebral blood circulation;
6. Unstable angina, myocardial infarction during the last 3 months;
7. Diseases (infectious, dermatological) accompanied by a pronounced chronic inflammation and purulent-septic complications;
8. Any somatic diseases in the stage of decompensation, mental disorder or alcoholism (daily consumption of more than 30 ml of alcohol during the last 3 months), drug addiction;
9. Significant emotional and behavioral disorders: severe depression (total score on the Beck Depression Inventory > 20 points), high anxiety (total score on the Spielberger-Hanin scale > 45 points);
10. The use of drugs that have a potentially negative effect on intellectual and cognitive functions (neuroleptics, tricyclic antidepressants, benzodiazepines, central cholinolytics, barbiturates, antiepileptic drugs);
11. Presence of contraindications to the administration of antiarrhythmic drugs and their components; any other condition that required therapy that, as indicated in the instructions for the drugs, could pose a risk to a patient or conflict with the purpose of the study.
All participants were divided into 2 groups depending on the prescribed therapy: group 1 (rhythm control) — 87 people who underwent pharmacological cardioversion with amiodarone to restore sinus rhythm; group 2 (heart rate control) — 29 patients who did not restore sinus rhythm due to contraindications (resistant AF, duration of AF more than 1 year, left atrial enlargement more than 50 mm, inability to maintain sinus rhythm despite cardioversion and adequate antiarrhythmic therapy, thyroid pathology with impaired function of the gland).
Pharmacological cardioversion with amiodarone: intravenous bolus 5 mg/kg body weight for 10–15 minutes in 5% glucose solution or intravenously for 30–60 minutes per 200 ml of polarizing mixture. If the paroxysmal AF was not controlled, amiodarone was prescribed in a tablet form: 1.2 g per day in 3 doses up to a total dose of 10 g, followed by a maintenance dose. The QT interval was observed on the electrocardiogram. When the interval was prolonged by 10–15 %, the maintenance dose was changed.
Patients of group 2 received drug therapy aimed at achieving normosystole. Therapy with metoprolol at a daily dose of 50–200 mg, then at a maintenance dose of 25–100 mg was received by 20 patients. Amiodarone according to the scheme 800 mg/day for 1 week orally, 600 mg/day for 1 week, 400 mg/day for 4 weeks, then at a maintenance dose of 200 mg/day orally was administered to 6 people. Therapy with digoxin 0.5 mg orally, then at a maintenance dose of 0.125–0.375 mg/day orally was received by 3 patients. Heart rate was considered controlled if it was 60–80 per minute at rest and 90–115 per minute during moderate-intensity physical activity.
The research protocol included a washout period — nootropic, vascular drugs were discontinued 14 days before inclusion in the study. At the time of the study, patients were receiving therapy that included, as indicated, antihypertensive, antithrombotic and hypolipidemic drugs.
AF before admission to the hospital was detected in 89 (76.7 %) patients and its duration ranged from 1 hour to 14 days. Sinus rhythm was restored in 73 (83.9 %) cases. Among patients with an arrhythmia lasting less than 48 hours, sinus rhythm was restored in 55 (84.6 %) individuals. After restoration of sinus rhythm on the background of a maintenance dose of amiodarone, 5 patients had relapses of AF, which were controlled by additional administration of amiodarone. Prophylactically amiodarone was prescribed in 100 % of cases.
Among 14 patients in whom sinus rhythm was not restored with amiodarone, 11 had severe coronary heart di-sease (angina pectoris III–IV functional class, postinfarction cardiosclerosis), 7 — mitral stenosis, 5 — thyroid pathology. Subsequently, in 4 patients the sinus rhythm was restored by electrical cardioversion; in 1 person after another recurrence of AF, it was decided not to restore the rhythm. No adverse reactions to amiodarone were noted.
Evaluation of the effectiveness of pharmacological cardioversion was based on the dynamics of neurological symptoms and cognitive functions, indicators of central and cerebral hemodynamics, markers of systemic inflammation and was performed 10 days after the restoration of sinus rhythm.
Clinical and neurological examination included clarification of complaints with an emphasis on impaired memo-ry, attention, speech and other cognitive functions, emotional instability. Objective neurological examination was performed according to the generally accepted method. A formalized score was used to assess the severity of symptoms. The absence of a symptom was given 0 points, a mild symptom — 1, a moderate symptom — 2, and a severe symptom — 3 points. After treatment, the patient assessed the severity of the corresponding complaints according to the following scheme: 3 points — a symptom remained at the previous level, 2 points — the severity of a symptom decreased, 1 point — a symptom decreased significantly and 0 points — a symptom regressed. If a symptom worsened during therapy, 4 points were given.
Neuropsychological examination included the following tests: MMSE (Folstein M. et al., 1975), FAB (Dubois B. et al., 2000), DRS (Mattis S., 1976), 10 words (Luria A.R., 1969), 5 words (Grober E. et al., 1988), verbal association (Kazdin A., 1982), Judgment of Line Orientation (Benton A., 1975), unpainted objects (Luria A.R., 1969), clock drawing (Sunderland T. et al., 1989), test of connection of numbers and letters (Trail Making Test) (Reitan R.M., 1958), Boston Naming Test (Kaplan J. et al., 1978), Spielberger-Hanin anxiety self-assessment scale (Spielberger C.D. et al., 1976), Beck Depression Inventory (Beck A.T. et al., 1975) [7].
The study of central hemodynamics consisted of two-dimensional transthoracic echocardiography in the pulsed wave tissue Doppler mode using an ultrasound scanner Logiq 500 MD (Japan) according to standard methods. Cerebral hemodynamics, ultrasound dopplerography were evaluated on MyLab 25 device (Esaote S.p.A., Italy) accor-ding to standard methods. The blood flow velocities (peak systolic (Vps), end-diastolic (Ved), mean (Vm)) and indices of vascular resistance (pulsatility index (PI) and resistive index (RI)) in the middle cerebral artery were studied.
To assess the inflammatory profile, the blood levels of cytokines (tumor necrosis factor α (TNF-α), interleukin-6 (IL-6)) were determined by enzyme-linked immunosorbent assay on a biochemical analyzer Immulite 1000 (Siemens AG, Germany). The level of С-reactive protein (CRP) was evaluated by immunoturbidimetric method on the biochemical analyzer Cobas Integra 400 plus (Roche, Switzerland).
The results of statistical processing of quantitative variables are represented by the means and standard deviations (M ± SD). The study used application packages Statistica for Windows v.8.0 (StatSoft Inc., USA, 2012) in accordance with the recommendations for processing the results of biomedical research.
Results and discussion
Patients in both groups had an average of 4–5 complaints on the background of paroxysmal AF. In group 1, the overall score of complaints was 12.3 ± 2.3 points, in group 2 — 12.1 ± 2.2 points (p = 0.95). Patients of group 1 after successful pharmacological cardioversion and people of group 2 after achieving normosystole reported an improvement in well-being: a decrease in headache, vertigo, noise in the head, irritability, general weakness, improved ability to concentrate, sleep. However, group 1 patients noted a decrease in the intensity of most complaints by 49.6 % (p = 0.031), in group 2 — by 13.2 % compared to baseline (p = 0.58). Thus, following therapy, representatives of group 1 assessed their condition more favorably than patients of group 2 (Fig. 1).
/32.jpg)
Group 1 had a regression of the following syndromes: cephalgic — from 2.1 ± 0.6 to 0.6 ± 0.2 points (p = 0.019), vestibulo-atactic — from 2.4 ± 0.6 to 0.8 ± 0.2 (p = 0.012), cochleovestibular — from 2.0 ± 0.5 to 0.6 ± 0.2 (p = 0.01), dissomnic — from 2.3 ± 0.6 to 0.8 ± 0.2 (p = 0.019), paro-xysmal — from 2.0 ± 0.5 to 0 points (p < 0.001). The analysis of indicators of group 2 also revealed a regression of neurological symptoms, but it was unreliable. Thus, the cephalgic syndrome decreased from 2.0 ± 0.5 to 1.5 ± 0.4 points (p = 0.44), vestibulo-atactic — from 2.3 ± 0.6 to 1.8 ± 0.5 (p = 0.52), cochleovestibular — from 1.8 ± 0.5 to 1.5 ± 0.4 (p = 0.64), dissomnic — from 2.1 ± 0.5 to 1.6 ± 0.4 (p = 0.44), paroxysmal — from 1.8 ± 0.5 to 1.3 ± 0.3 points (p = 0.39). The dynamics of other syndromes was absent (Fig. 2).
/33.jpg)
The most noticeable effect of antiarrhythmic therapy in relation to neurological symptoms was observed for such manifestations of cerebrovascular insufficiency as cephalgia, vertigo, instability, fainting, reduced efficiency. Patients of group 1 observed a more pronounced regression of neurological and cardiac symptoms compared with group 2.
The subjective clinical effect of therapy on neurological complaints in most patients was manifested on days 3–4 of treatment. In group 1 after 10 days, a significant improvement was observed in 27.6 % of cases, moderate — in 33.3 %, insignificant — in 20.7 %, and 18.4 % of patients had no changes. The following results were obtained in group 2: a moderate improvement — 24.1 % of cases, insignificant — 31.0 %, no changes — 34.6 %, deterioration — 10.3 % (Fig. 3).
Thus, the analysis of treatment effectiveness showed that in group 1, positive results were obtained for 81.9 % of people, in group 2 — for 55.1 %.
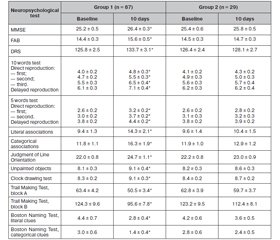
In patients of group 1, the MMSE score increased by 4.5 % (p = 0.041), FAB — by 7.7 % (p = 0.041), in group 2 — by 1.5 % (p = 0.61) and 1.4 % (p = 0.64), respectively. The positive dynamics of most subtests in group 1 was significant compared to group 2 (Table 1).
In patients of group 1, the result for DRS increased by 5.9 % (p = 0.049), in group 2 — by 1.3 % (p = 0.64). Positive dynamics (p = 0.43) in group 1 was considered unreliable only for the subtest “constructive praxis”, on other subtests, the differences from the baseline indicators were significant (p < 0.05). In patients of group 2, for all DRS subtests an improvement was insignificant (p = 0.62) (Table 1).
Auditory-speech and visual memory improved in both groups, but in group 1, direct and delayed reproductions on retesting were significantly higher than in group 2 (p < 0.05) (Table 1).
The results of tests to assess the speaking rate in patients of group 1 were significantly better than in group 2: the indicator of the test “literal associations” in group 1 increased by 34.3 % (p = 0.049); “categorical associations” — by 27.6 % (p = 0.042). In group 2, the positive dynamics of these indicators was unreliable (Table 1).
Performance of Judgment of Line Orientation and recognition of unpainted objects improved in both groups compared to the baseline, but in group 1, the results of both tests were significantly better (p < 0.05). The result of Judgment of Line Orientation in group 1 after 10 days of treatment increased by 10.9 % (p = 0.049), in group 2 — by 3.5 % (p = 0.51). Thus, in group 1, patients noted a significant improvement in visual-spatial gnosis. A similar trend was found when studying simultaneous gnosis: in group 1, it increased by 11 % (p = 0.047), in group 2 — by 4.6 % (p = 0.89).
Patients of group 1 performed the clock drawing test significantly better compared to the baseline — by 8.8 % (p = 0.028). In group 2, an improvement was insignificant — 3.4 % (p = 0.29).
The focus scores on the Trail Making Test in group 2 improved significantly less than in group 1. Performance on block A in patients of group 1 in the dynamics decreased by 20.3 % (p = 0.018), in group 2 — by 4.9 % (p = 0.57); on block B — by 23.1 % (p = 0.021) and 8.8 % (p = 0.39), respectively.
Nominative speech function in patients of group 1 restored significantly better: the frequency of literal clues when performing the Boston Naming Test in group 1 decreased by 36.4 % (p = 0.049), in group 2 — by 14.3 % (p = 0.44); the frequency of categorical clues in group 1 decreased by 53.3 % (p = 0.028), in group 2 — by 14.3 % (p = 0.61).
We found an improvement of the emotional background: in patients of group 1, reactive anxiety decreased significantly — by 21.6 % (p = 0.048), depression — by 15.1 % (p = 0.043). Depressive symptoms regressed in 22 (25.3 %) patients. In group 2, the dynamics of affective disorders was insignificant: reactive anxiety decreased by 5.4 % (p = 0.60), depression — by 2.8 % (p = 0.71) (Table 2).
Thus, against the background of the restoration of sinus rhythm, a significant improvement in memory, attention, speaking rate, visual-spatial and simultaneous gnosis, speech activity, as well as emotional status was noted. Following the-rapy aimed at controlling heart rate, there was also a positive trend, but the differences from baseline were insignificant.
In both groups, there was a decrease in end-diastolic, end-systolic volume and an increase in left ventricular ejection fraction, but in group 1, normalization of these indicators was significant, and the left atrial size on the background of sinus rhythm restoration decreased to the level that did not exceed the norm. In patients of group 1 on the background of treatment, there was a significant increase in the left ventricular ejection fraction by 10.7 % (p = 0.033), in group 2 — by 1.2 % (p = 0.81). In both groups, there was a decrease in mean values of minute volume and an increase in total peripheral vascular resistance: in group 1 — by 38 % (p = 0.032) and 32.7 % (p = 0.042), in group 2 — by 25.3 % (p = 0.20) and 24.3 % (p = 0.14), respectively (Table 3).
Thus, the changes in the parameters of echocardiography were determined primarily by the actual restoration of rhythm and a decrease in heart rate. At the same time, there was a clear positive dynamics of most indicators of central hemodynamics and myocardial contractility. Changes in rhythm recovery were more pronounced compared with the strategy of controlling heart rate.
In patients of group 1, a significant increase in hemodynamic indicators of the middle cerebral artery was registered: Vps — by 8.3 % (p = 0.049), Ved — by 20.6 % (p = 0.002), Vm — by 14 % (p = 0.048), as well as a decrease in vascular resistance: RI — by 9.7 % (p = 0.035), PI — by 15.1 % (p = 0.042). In group 2, there were insignificant changes of all velocity characteristics of the middle cerebral artery (p > 0.05) (Table 4).
Thus, successful pharmacological cardioversion led to improved cerebral hemodynamics in the middle cerebral artery, which slowed the progression of cognitive disorders.
Cytokine levels decreased statistically significantly in patients of group 1: TNF-α — by 29.7 % (p = 0.048), IL-6 — by 28.1 % (p = 0.049), but the positive dynamics of CRP was insignificant (p = 0.13). In group 2, all indicators had only a tendency to decrease (p > 0.05) (Table 5).
Thus, the positive clinical dynamics in the process of sinus rhythm restoration was associated with a statistically significant decrease in the content of proinflammatory cytokines, which indicated a decrease in the activity of immune inflammation.
Restoration of sinus rhythm improves neurological symptoms, helps reduce the severity of cognitive and affective disorders in patients with paroxysmal AF by reducing hypersympathicotonia, improving systolic and diastolic characteristics of the left ventricle, left ventricular contracti-
lity, central hemodynamics, functional state of cerebral blood flow, reducing the activity of immune inflammation.
Our data suggest that the restoration of sinus rhythm has a number of significant advantages over the strategy of heart rate control, as it leads to a significant improvement in cognitive functions. These data are inconsistent with the results of meta-analyzes, which do not show the advantages of sinus rhythm maintenance tactics over heart rate control in patients with paroxysmal AF. Our study proved the added benefit of successful pharmacological cardioversion, which is of great practical importance.
Conclusions
1. In patients who achieved restoration of sinus rhythm, a more pronounced regression of neurological symptoms was observed compared to the rhythm control group. The most noticeable effect of antiarrhythmic therapy in relation to neurological symptoms was observed for such manifestations of cerebrovascular insufficiency as cephalgia, vertigo, instability, fainting, reduce efficiency.
2. Against the background of sinus rhythm restoration, a significant improvement in all cognitive functions was noted: memory, attention, speaking rate, visual-spatial and simultaneous gnosis, speech activity, as well as emotional status.
3. The improvements in the parameters of central and cerebral hemodynamics were determined primarily by the actual restoration of rhythm and a decrease in heart rate. Changes in rhythm recovery were more pronounced compared to the strategy of heart rate control.
4. Positive clinical dynamics in the process of sinus rhythm restoration was associated with a statistically significant decrease in the content of proinflammatory cytokines, which indicated a decrease in the activity of immune inflammation.
5. Successful pharmacological cardioversion with amiodarone has an optimizing effect on the neurological and cognitive functions of patients with paroxysmal atrial fibrillation due to improved left ventricular contractility, functional state of cerebral blood flow and reduced immune inflammation activity.
Received 01.10.2022
Revised 12.10.2022
Accepted 24.10.2022
/32.jpg)
/33.jpg)

/33_2.jpg)
/34.jpg)
/35.jpg)