Международный эндокринологический журнал Том 16, №2, 2020
Вернуться к номеру
Very severe hypertriglyceridemia in a subject with poor glycemic control: a case report with general consideration
Авторы: E. Xhardo, F. Agaçi
Department of Internal Medicine, University Hospital “Shefqet Ndroqi”, Tirana, Albania
Рубрики: Эндокринология
Разделы: Справочник специалиста
Версия для печати
Гіпертригліцеридемія визначається як рівень тригліцеридів сироватки крові натще понад 150 мг/дл. Сучасна класифікація включає легку та помірну, тяжку та дуже тяжку гіпертригліцеридемію. Легка й помірна гіпертригліцеридемія підвищує ризик серцево-судинних подій, тоді як тяжка й різко виражена є фактором ризику гострого панкреатиту. Звичайна фармакотерапія гіпертригліцеридемії включає фібрати, ніацин, статини, езетиміб, омега-3 жирну кислоту. Інші способи, які дозволяють знизити рівень тригліцеридів, представлені плазмаферезом та терапією ліпопротеїновою ліпазою. Описаний клінічний випадок 55-річного чоловіка без анамнезу родинного цукрового діабету (ЦД), дисліпідемії, ранньої ішемічної хвороби серця. ЦД 2-го типу діагностований у 2016 році; із 2018 року пацієнт отримує інсулінотерапію. В анамнезі: артеріальна гіпертензія протягом приблизно 15 років, хронічна хвороба нирок, різко виражена гіпертригліцеридемія, хронічна обструктивна хвороба легень. Пацієнт дотримувався лікування гіпоглікемічною, гіполіпідемічною дієтою з низьким умістом солі, препаратами фібратів, статинів, омега-3 жирної кислоти.
Гипертриглицеридемия определяется как уровень триглицеридов сыворотки крови натощак более 150 мг/дл. Современная классификация включает легкую и умеренную, тяжелую и очень тяжелую гипертриглицеридемию. Легкая и умеренная гипертриглицеридемия повышает риск сердечно-сосудистых событий, тогда как тяжелая и резко выраженная является фактором риска острого панкреатита. Обычная фармакотерапия гипертриглицеридемии включает фибраты, ниацин, статины, эзетимиб, омега-3 жирные кислоты. Другие способы, которые позволяют снизить уровень триглицеридов, представлены плазмаферезом и терапией липопротеиновой липазой. Описан клинический случай 55-летнего мужчины без анамнеза семейного сахарного диабета (СД), дислипидемии, ранней ишемической болезни сердца. СД 2-го типа диагностирован в 2016 году; с 2018 года пациент получает инсулинотерапию. В анамнезе артериальная гипертензия в течение примерно 15 лет, хроническая болезнь почек, резко выраженная гипертриглицеридемия, хроническая обструктивная болезнь легких. Пациент придерживался лечения гипогликемической, гиполипидемической диетой с низким содержанием соли, препаратами фибратов, статинов, омега-3 жирной кислоты.
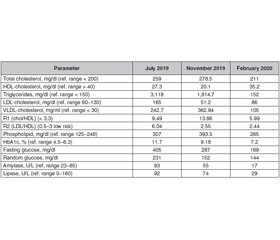
Hypertriglyceridemia is defined as a value of fasting serum triglyceride over 150 mg/dl. The classification of hypertriglyceridemia according to the Endocrine Society includes mild and moderate hypertriglyceridemia, severe hypertriglyceridemia and very severe hypertriglyceridemia. Mild and moderate hypertriglyceridemia increases the risk for cardiovascular events while severe and very severe hypertriglyceridemia is a risk factor for acute pancreatitis. Conventional pharmacological therapy of hypertriglyceridemia includes fibrates, niacin, statins, ezetimibe, and omega-3 fatty acid. Other triglyceride-lowering therapies are represented by plasmapheresis and lipoprotein lipase gene therapy. The present work refers to a 55-year-old man without a history of family diabetes mellitus (DM), dyslipidemia, premature coronary artery disease, diagnosed with type 2 DM in 2016, from 2018 on insulin treatment; he was hospitalized for endocrine evaluation. The patient had a history of high blood pressure for approximately 15 years, chronic kidney disease, very severe hypertriglyceridemia, and chronic obstructive pulmonary disease. The patient followed treatment with hypoglycemic, hypolipemic, low-salt diet, fibrates, statins, omega-3 fatty acid.
різко виражена гіпертригліцеридемія; цукровий діабет; лікування
резко выраженная гипертриглицеридемия; сахарный диабет; лечение
very severe hypertriglyceridemia; diabetes mellitus; treatment
Introduction
General considerations
Case report
Treatment of hypertriglyceridemia
Conclusions
- Berglund L., Brunzell J.D., Goldberg A.C. et al. Evaluation and Treatment of Hypertriglyceridemia: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2012. 97 (9). 2969-2989.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001. 285 (19). 2486-2497.
- Yuan G., Al-Shali K., Hegele R.A. Hypertriglyceridemia: its etiology, effects and treatment. Can. Med. Assoc. J. 2007. 176 (8). 1113-1120.
- Bouabdellah M., Iraqi H., Benlian P. et al. Familial hypertriglyceridemia: biochemical, clinical and molecular study in a Moroccan family. Ann. Biol. Clin. 2015. 73 (4). 474-484.
- Bainton D., Miller N.E., Bolton C.H. et al. Plasma triglyceride and high-density lipoprotein cholesterol as predictors of ischaemic heart disease in British men: The Caerphilly and Speedwell Collaborative Heart Disease Studies. Br. Heart J. 1992. 68 (1). 60-66.
- Abdel-Maksoud M.F., Hokanson J.E. The complex role of triglycerides in cardiovascular disease. Semin. Vasc. Med. 2002. 2 (3). 325-333.
- Patel A., Barzi F., Jamrozik K. et al. Serum Triglycerides as a Risk Factor for Cardiovascular Diseases in the Asia-Pacific Region. Circulation. 2004. 110 (17). 2678-2686.
- Tirosh A., Rudich A., Shochat T. et al. Changes in Triglyceride Levels and Risk for Coronary Heart Disease in Young Men. Ann. Intern. Med. 2007. 147 (6). 377-385.
- Hokanson J.E., Austin M.A. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J. Cardiovasc. Risk. 1996. 3 (2). 213-219.
- Kannel W.B., Vasan R.S. Triglycerides as vascular risk factors: New Epidemiologic Insights for Current Opinion in Cardiology. Curr. Opin. Cardiol. 2009. 24 (4). 345-350.
- Gan S.I., Edwards A.L., Symonds C.J., Beck P.L. Hypertriglyceridemia-induced pancreatitis: A case-based review. World J. Gastroenterol. 2006. 12 (44). 7197-7202.
- Yang F., Wang Y., Sternfeld L. et al. The role of free fatty acids, pancreatic lipase and Ca2+ signaling in injury of isolated acinar cells and pancreatitis model in lipoprotein lipase-deficient mice. Acta Physiol. (Oxf). 2009. 195 (1). 13-28.
- Sztefko K., Panek J. Serum free fatty acid concentration in patients with acute pancreatitis. Pancreatology. 2001. 1 (3). 230-236.
- De Beaux A.C., Ross J.A., Maingay J.P. et al. Proinflammatory cytokine release by peripheral blood mononuclear cells from patients with acute pancreatitis. Br. J. Surg. 1996. 83. 1071-1075.
- Kusnierz-Cabala B., Gurda-Duda A., Dumnicka P. et al. Analysis of selected inflammatory markers for early prediction of severe clinical course of acute pancreatitis. Przegl. Lek. 2013. 70. 392-396.
- Kota S.K., Kota A.K., Jammula S. et al. Hypertriglyceridemia-induced recurrent acute pancreatitis: A case-based review. Indian J. Endocrinol. Metab. 2012. 16 (1). 141-143.
- Barter P.J., Rye K.A. Cardioprotective properties of fibrates: Which fibrate, which patients, what mechanism? Circulation. 2006. 113. 1553-1555.
- Carlson L.A. Nicotinic acid: the broad-spectrum lipid drug. A 50th anniversary review. J. Intern. Med. 2005. 258. 94-114.
- Bays H. Ezetimibe. Expert Opin. Investig. Drugs. 2002. 11 (11). 1587-604.
- Hooper L., Thompson R.L., Harrison R.A. et al. Risks and benefits of omega 3 fats for mortality, cardiovascular disease and cancer: Systematic review. BMJ. 2006. 332. 752-760.
- Shearer G.C., Savinova O.V., Harris W.S. Fish oil — how does it reduce plasma triglycerides? Biochim. Biophys. Acta. 2012. 1821 (5). 843-851.

/98.jpg)