Международный эндокринологический журнал Том 17, №1, 2021
Вернуться к номеру
Клінічна характеристика пацієнтів з COVID-19: ретроспективне дослідження у Саудівській Аравії
Авторы: Marwah Bin Talib(1), Abdullah A. Baredhwan(2), Khaled Alenazi(2), Ali Almagooshi(2), Abdulrehman M. Alqahtani(2), Sultan A. Alsobayeg(2), Sarah Alhazmi(2), Waad Awad(2), Ameera S. Alamri(2), Parameaswari P. Jaganathan(2), Manasik N. Abdu(3), Latif Ahmed Khan(2)
(1) — King Faisal Specialist Hospital, Kingdom of Saudi Arabia
(2) — King Saud Medical City, Riyadh, Kingdom of Saudi Arabia
(3) — College of Medicine, Al-Faisal University, Riyadh, Saudi Arabia
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
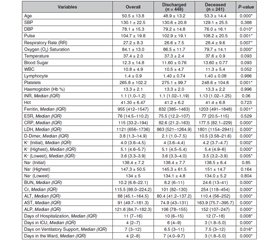
Актуальність. У Китаї вперше повідомили про вірусне захворювання COVID-19, спричинене коронавірусом (SARS-CoV-2). Всесвітня організація охорони здоров’я оголосила пандемію COVID-19 в березні 2020 року. Спостерігається значна кількість випадків цієї хвороби, яка стала тягарем для систем охорони здоров’я і призвела до високої летальності. Ціль. Дослідження сплановане з метою встановити особливості клінічної картини захворювання, ведення хворих і кінцеві результати лікування COVID-19 у популяції Королівства Саудівська Аравія та порівняти показники з іншими установами. Матеріали та методи. Ретроспективне дослідження пацієнтів із COVID-19 з тяжким перебігом і критичними станами було проведене в медичному центрі Ер-Ріяду. Дозвіл на його проведення виданий комітетом з етики медичного центру. Клінічні дані зібрані з електронних записів пацієнтів. Показники 689 пацієнтів, які зверталися за допомогою з 1 березня 2020 року по 30 червня 2020 року, аналізували за допомогою стандартних статистичних методів. Результати. Понад 50 % пацієнтів (середній вік 50 років) були з Індійського субконтиненту (Індія, Пакистан і Бангладеш). Жінки становили 17,3 % обстежених. Поширеними явищами у хворих були задишка (79 %), кашель (70 %) і лихоманка (67 %). Середня насиченість крові киснем у них становила 92 %. Приблизно 61 % пацієнтів перебували в критичному стані та лікувались у відділенні інтенсивної терапії. Смертність становила 35 %, а поліорганна недостатність — 25 %. Цукровий діабет належав до найчастіших супутніх станів (37,3 %), як і артеріальна гіпертензія (29,5 %). При цьому їх наявність не призводила до збільшення летальності цих пацієнтів. Показник летальності, очевидно, пов’язаний із несвоєчасним зверненням до медичних закладів та тяжкістю самої хвороби. Висновки. Наведені результати ретроспективного дослідження за участю 689 пацієнтів із тяжким перебігом COVID-19 свідчать про високу частку госпіталізацій у відділення інтенсивної терапії — 60,8 %. З цього числа 41 % хворих потребували інвазивної вентиляції легень, 29 % — використання препаратів вазопресивної дії та 14 % — проведення гемодіалізу. Смертність становила 35 %. Понад 50 % хворих становили вихідці з Індійського субконтиненту.
Актуальность. В Китае впервые сообщили о вирусном заболевании COVID-19, вызванном коронавирусом (SARS-CoV-2). Всемирная организация здравоохранения объявила пандемию COVID-19 в марте 2020 года. Наблюдается значительное количество случаев этой болезни, которая стала бременем для систем здравоохранения и привела к высокой летальности. Цель. Исследование спланировано с целью установить особенности клинической картины заболевания, ведения больных и конечные результаты лечения COVID-19 в популяции Королевства Саудовская Аравия и сравнить показатели с другими учреждениями. Материалы и методы. Ретроспективное исследование пациентов с COVID-19 с тяжелым течением и критическими состояниями было проведено в медицинском центре Эр-Рияда. Разрешение на его проведение выдано комитетом по этике медицинского центра. Клинические данные собраны из электронных записей пациентов. Показатели 689 пациентов, обращавшихся за помощью с 1 марта 2020 по 30 июня 2020 года, анализировали с помощью стандартных статистических методов. Результаты. Более 50 % пациентов (средний возраст 50 лет) были с Индийского субконтинента (Индия, Пакистан и Бангладеш). Женщины составляли 17,3 % обследованных. Распространенными явлениями у больных были одышка (79 %), кашель (70 %) и лихорадка (67 %). Средняя насыщенность крови кислородом у них составляла 92 %. Примерно 61 % пациентов находились в критическом состоянии и лечились в отделении интенсивной терапии. Смертность составляла 35 %, а полиорганная недостаточность — 25 %. Сахарный диабет принадлежал к наиболее частым сопутствующим состояниям (37,3 %), как и артериальная гипертензия (29,5 %). При этом их наличие не приводило к увеличению летальности этих пациентов. Показатель летальности, очевидно, связан с несвоевременным обращением в медицинские учреждения и тяжестью самой болезни. Выводы. Приведенные результаты ретроспективного исследования с участием 689 пациентов с тяжелым течением COVID-19 свидетельствуют о высокой доле госпитализаций в отделение интенсивной терапии — 60,8 %. Из этого числа 41 % больных нуждались в инвазивной вентиляции легких, 29 % — в использовании препаратов вазопрессивного действия и 14 % — в проведении гемодиализа. Смертность составляла 35 %. Более 50 % больных составляли выходцы с Индийского субконтинента.
Background. COVID-19, a new viral disease caused by Corona Virus (SARS-CoV-2) was reported first by Chinese. WHO declared it a pandemic in March 2020. We saw a huge number of this illness that caused a stress on health care systems and a high proportion of mortality. World Health Organization declared it as a pandemic in March 2020. We planned this study with the objective of knowing clinical presentation, hospital management and final outcome of COVID-19 in our population and compare it with other institution who studied the disease elsewhere. Materials and methods. A retrospective study on COVID-19 patients with severe to critical illness was conducted in King Saud Medical City Riyadh. Proper permission was issued by ethical committee of King Saud Medical City. Data was collected manually as well from electronic records. Data was analyzed using standard statistical methods. A total of 689 patients that were admitted to KSMC from 1st March 2020 to 30th of June 2020. Results. More than 50 % of our patients were from Indian subcontinent (India, Pakistan and Bangladesh). Our mean age was 50 years. Females comprised 17.3 % of our patients. Common presentation was breathlessness (79 %), cough (70 %) and fever (67 %). Mean oxygen saturation on presentation was 92 %. Around sixty one percent of our patients were critical and were treated in intensive care unit. Mortality was 35 % and multi-organ failure 25 %. Although diabetes mellitus (37.3 %) and hypertension (29.5 %) were common comorbidities but it did not increase the mortality in our patients. Our mortality seems to be related to late reporting to hospital and severe disease itself. Conclusions. A retrospective study conducted at King Saud Medical city on 689 patients of severe and critical COVID-19. A high proportion were admitted to intensive care unit (60.8 %), 41 % needed invasive ventilation and 29 % required vasopressors and 14 % needed hemodialysis. Mortality of 35 % was recorded in our study. People of Indian subcontinent (Pakistani, Bangladeshi and Indians) formed more than 50 % of patients.
COVID-19; цукровий діабет; артеріальна гіпертензія; Королівство Саудівська Аравія
COVID-19; сахарный диабет; артериальная гипертензия; Королевство Саудовская Аравия
COVID-19; diabetes mellitus; hypertension; Kingdom of Saudi Arabia
Introduction
Materials and methods
Results
Discussion
Conclusions
Acknowledgement
- Novel Coronavirus (2019-nCoV). World Health Organization WHO 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [2020-1-24].
- Tan W., Zhao X., Ma X., Wang W., Niu P., Xu W. et al. A Novel Coronavirus Genome Identified in a Cluster of Pneumonia Cases — Wuhan, China 2019−2020. China CDC Weekly. 2020. 2(4). 61-62. DOI: 10.46234/ccdcw2020.017.
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020. 76. 71-76. doi: 10.1016/j.ijsu.2020.02.034.
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020. 395(10224). 565-574. doi: 10.1016/S0140-6736(20)30251-8.
- Pal M., Berhanu G., Desalegn C., Kandi V. Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): An Update. Cureus. 2020. 2(3). doi: 10.7759/cureus.7423.
- Wu Z., McGoogan J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. J. Am. Med. Assoc. 2020. 323(13). 1239-1242. doi: 10.1001/jama.2020.2648.
- Oran D.P., Topol E.J. Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review. Ann. Intern. Med. 2020. 173(5). 362-367. doi: 10.7326/M20-3012.
- Lavezzo E., Franchin E., Ciavarella C., Gina Cuomo-Dannenburg G., Barzon L., Claudia Del Vecchio C., Rossi L., Manganelli R. et al. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature. 2020. 584. 425-429. https://doi.org/10.1038/s41586-020-2488-1.
- Gideon Meyerowitz-Katz G., Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. International Journal of Infectious Diseases. 2020. 101. 138-148. https://doi.org/10.1016/j.ijid.2020.09.1464.
- Alsofayan Y.M., Althunayyan S.M., Khan A.A., Hakawi A.M., Assiri A.M. Clinical characteristics of COVID-19 in Saudi Arabia: A national retrospective study. J. Infect. Public Health. 2020. 13(7). 920-925. doi: 10.1016/j.jiph.2020.05.026.
- COVID-19 Dashboard: Saudi Arabia. https://covid19.moh.gov.sa/ (accessed Nov. 29, 2020).
- Saudi MoH Protocol for Patients Suspected of/Confirmed with COVID-19 Supportive care and antiviral treatment of suspected or confirmed COVID-19 infection. Accessed: Dec. 09, 2020. [Online]. Available: https://covid19.cdc.gov.sa/.
- Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., Wu Y. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020. 8(5). 475-481. doi: 10.1016/S2213-2600(20)30079-5.
- Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K., Greninger A.L. et al. COVID-19 in Critically Ill Patients in the Seattle Region — Case Series. N. Engl. J. Med. 2020. 382(21). 2012-2022. doi: 10.1056/nejmoa2004500.
- Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H. et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020. 180(7). 934-943. doi: 10.1001/jamainternmed.2020.0994.
- Barry M., AlMohaya A., AlHijji A., Akkielah L., AlRajhi A., Almajid F., Alsharidi A. et al. Clinical Characteristics and Outcome of Hospitalized COVID-19 Patients in a MERS-CoV Endemic Area. J. Epidemiol. Glob. Health. 2020. 2020. doi: 10.2991/jegh.k.200806.002.
- Tamara A., Tahapary D.L. Obesity as a predictor for a poor prognosis of COVID-19: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2020. 14(4). 655-659. doi: 10.1016/j.dsx.2020.05.020.
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B. et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020. 323(11). 1061-1069. doi: 10.1001/jama.2020.1585.
- Flythe J.E., Assimon M.M., Tugman M.J., Chang E.H., Gupta S., Shah J., Sosa M.A. et al.; STOP-COVID Investigators. Characteristics and Outcomes of Individuals With Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States. Am. J. Kidney Dis. 2021. 77(2). 190-203.e1. doi: 10.1053/j.ajkd.2020.09.003. Epub 2020 Sep 19.
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. J. Am. Med. Assoc. 2020. 323(20). 2052-2059. doi: 10.1001/jama.2020.6775.
- Onder G., Rezza G., Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020. 323(18). 1775-1776. doi: 10.1001/jama.2020.4683.
- Shabrawishi M., Al-Gethamy M.M., Naser A.Y., Ghazawi M.A., Alsharif G.F., Obaid E.F., Melebari H.A. et al. Clinical, radiological and therapeutic characteristics of patients with COVID-19 in Saudi Arabia. PLoS One. 2020. 15(8). e0237130. doi: 10.1371/journal.pone.0237130.
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., Liu L. et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020. 382(18). 1708-1720. doi: 10.1056/nejmoa2002032.

/13.jpg)
/14.jpg)