Introduction
The Importance of occupational health and safety
With the industrial revolution, the working population began to increase. Employees have faced dangerous and risky situations with job diversity, mechanization and changing working environment conditions based on industrialization and technological developments. These situations lead to the formation of physical and mental problems and an increase in occupational accidents, thus reducing productivity and economic loss. Today, the importance of occupational health and safety, which aims to eliminate or minimize all these negativities, is increasing rapidly. Activities carried out within the scope of occupational health and safety (OHS), employees. It includes protecting and increasing their health, safety, productivity and making the workplace suitable for healthy and safe working. The fact that the cost of the expenditures made to eliminate the damages caused by occupational accidents and occupational diseases is quite high is an element that shows how important OHS is [1].
Concepts of occupational accidents and missing event
An accident is an event that occurs unexpectedly and causes material and moral damage. The causes of most accidents are complex and result from a combination of multiple causes. Occupational accident, which is an unplanned and unexpected event that occurs in the workplace, results in physical or material damage to the person and the workplace [2].
Occupational accident is an event that causes physical or mental damage to the insured person, suddenly and with an external factor, due to the job or the necessity of the job while working with the employer [3].
For an incident to be called a work accident, the physical and/or mental integrity of the employee must be damaged [4].
Occupational accident is defined by WHO as an unplanned event that mostly leads to injuries, damage to machinery, tools and equipment, and stoppage of production for a while. The ILO has defined an occupational accident as an unplanned and unexpected event that causes certain damage or injury. In Article 3 of the Occupational Health and Safety Law, an occupational accident is defined as an event that occurs at the workplace or due to work, resulting in death or disrupting bodily integrity, causing mental or physical disability. In the Occupational Health and Safety Law No. 6331, the word “employee” is used for the person who has had a work accident in order to cover a wider employee base instead of the insured.
The conditions required for an incident to be qualified as an occupational accident are specified in the laws. In the Social Insurance and General Health Insurance Law No. 5510, the conditions required for the incident to be considered an occupational accident, the compensations to be paid after the accident in the Code of Obligations, and the penal responsibilities after the accident are specified in the Turkish Penal Code.
Social Insurance and General Health Insurance Law No. 5510 states that the following conditions must be met in order for an event to be considered as a work accident:
1. Insurance of the accident victim.
2. Being in the workplace or in one of the places specified in the law.
3. Immediate or subsequent bodily or mental harm to the person.
4. Finding a causal link between the accident and the result.
In the Occupational Health and Safety Risk Assessment Regulation; occurring in the workplace; it is defined as an event that does not cause harm even though it has the potential to cause damage to the employee, workplace or work equipment. According to statistics, 29 injury accidents occur in every 300 near-misses, and 1 fatal or severe injury accident occurs in every 29 injury accidents. In this respect, keeping near-miss records is of vital importance in order to prevent occupational accidents in the workplace. Near-miss studies on healthcare workers have not been found in our country, however, in one of the master’s thesis, the case of having a near-miss accident in a hospital was examined on nurses and 79.3 % of the nurses survived 1–2 times with a sharp object injury. Exposure to blood and body fluids was experienced by 64.8 % 1–2 times, 35.2 % 3 times or more. 70.2 % of the nurses survived the splash of blood and body fluid to the mucous membrane 1–2 times. On the other hand, 81.1 % of the nurses survived the slip and fall 1–2 times. 71.2 % of the nurses who narrowly survived the violence were exposed 1–2 times. The rate of those who survived a traffic accident 1–2 times on their way to and from work was found to be 80.6 % [5–7].
Importance of the subject in health institutions
Health institutions are considered occupational areas with high risk due to their need for human resources, including numerous specialists with distinct characteristics, use of intensive technology, and complex occupational processes. Besides, the health sector is mentioned as one of the riskiest occupational areas according to both our national legislation and previous literature on this subject, due to the risks and dangers faced by the employees while providing healthcare and, the nature of the service they provide [8]. The healthcare providers’ well-being, in terms of physical, psychological, and social aspects and a safe working environment, provide adequate health services, which are vital for health institutions. Healthcare professionals in high-risk hospitals must first ensure their safety and then focus on the safety of their patients, where they have to adopt and implement safety practices as a legal imperative and cultural change [9, 10]. Before occupational accidents occur, it is important to control the hazard at its source, design working systems ergonomically to minimize the risks, use personal protective equipment, and most importantly, emphasize the internalization of the subject by both management and employees [11, 12].
8.8 out of every 100 healthcare professionals working full-time in hospitals suffer from occupational accidents/occupational diseases or are removed from work. In comparison, this rate is 4 for every 100 employees in the mi-ning sector, 7.9 in the construction industry, and 8.1 in the production sector [13]. According to a study conducted in Germany in 2009, it is stated that healthcare professionals are exposed to physical and verbal violence throughout their professional life, with a lifetime risk of 70.7 % and 89.4 %, respectively [14, 15]. According to a study conducted by Turkish Health-Syndicate at the beginning of 2012 on 1864 healthcare professionals; 78 % of doctors and 69 % of nurses and midwives reported that they were exposed to violence [16, 17].
Health services are a risky sector in terms of occupational accidents. It is reported that the annual number of non-lethal occupational accidents are 262,700 in the USA; 16,548 in the UK and 35,491 in Canada. According to a study on accident types and occupations, which executed in the UK; large-scale injuries in nurses, assistant nurses, and caregivers were reported as slipping or snagging and assault or violence in 2002/2003. In a study conducted by the Ontario Occupational Health and Safety Insurance Department, it was found that 36,103 employees applied for work-related casualties, and 11 of them died between 1996 and 2000. According to a study examining the applications of the healthcare workers' insurance compensation in the USA, the most common reasons for application included sprains and muscle strains, crushing, bruises, cuts, and fractures [18–20].
The purpose of this study is to examine the frequency of exposure to occupational accidents and near-miss events of the nurses and physicians working in the internal medicine units of a university hospital, and their reporting status and factors affecting these characteristics.
Materials and methods
Type and objective of the research
This research, which aims to examine the frequency of exposure to occupational accidents and near-miss events, notification status and affecting factors of nurses and physicians working in the internal units of a university hospital, is descriptive and the data of the last 1 year were evaluated.
The aim of this study is to examine the frequency of exposure to occupational accidents and near-misses, notification status and the affecting factors of nurses and physicians working in the internal units of a university hospital.
Research Questions. What is the exposure to occupational accidents and near-misses in the last year according to the descriptive characteristics of health workers? Does exposure to work accident and near-miss incident have an effect with work history characteristics? Is there anyone who was exposed to work accidents and near-misses and did not report them? What are the reasons for not reporting?
Place and time of the research
The research was carried out in the internal units of a university hospital in Istanbul between 14.03.2018 and 07.05.2018. The hospital has 640 beds and consists of a total of 1484 employees, including 680 nurses and 355 physicians. In the internal units of this hospital, 111 nurses and 152 physicians provide treatment services.
The universe and sample of the research
Purposive sampling method, which is a non-probabilistic sampling type, was used in our research. The sampling criteria in the study are as follows.
Inclusion criteria:
— Working as a permanent or contracted physician, nurse in the Internal Units of the Hospital (internal intensive care, internal services) in January 01 — December 31, 2017.
— Volunteering to participate in the study.
Exclusion criteria:
— Being on annual leave.
— Temporary assignment to another unit.
Data collection tools
In the research, data were collected by using the “Occupational Accident and Near Miss Exposure Evaluation Form”. This form was created by the researchers. The form is structured in 4 sections and consists of questions prepared to describe the introductory work story characteristics, work accident and features of the employees, and near-miss event features. The form was created by the researcher considering the variables stated in the literature and thought to be effective regarding work accidents and near-misses in hospitals. In terms of the scope of the form and the clarity of the questions, it was presented to academicians who are experts in the field of occupational health and safety, internal medicine nursing and nursing research, and the form was finalized in line with the feedback.
Variables of the study
Dependent variables. Total accident rate and near-miss rate in the last 1 year.
Independent variables. Gender and age of physicians and nurses, Educational status, Duration of occupation, Unit and duration of work, Weekly working time, Status and number of work on duty, Occupational accidents and trai-ning on protection methods.
Research ethics
Prior to the research, institutional permission from Health Sciences University Göztepe Training and Research Hospital, Ethics Committee Approval from Üsküdar University Non-Invasive Research Ethics Committee was obtained. Also The Internal medicine service Clinic Chief and Supervisor Nurse were informed. The patients provided voluntary informed consent form in written.
Data collection
The data were collected by using face-to-face interview method during working hours, taking into account the service shift list, with the knowledge of the doctors and nurses in charge of the service, between 14.03.2018 and 07.05.2018, after obtaining the institutional permission and ethical permission. It took approximately 5 minutes for each participant to complete the data collection tools. The data form was prepared by the researcher by scanning the relevant literature. The data were collected with the “Assessment of Exposure to Work Accident and Near-Miss Incident” questionnaire consisting of 15 questions.
Data analysis and evaluation
The data were collected after receiving the institutional and ethical permissions by using the face-to-face interview method within the working hours by considering the service shift list and within the knowledge of the supervisor doctors and nurses. Hospital managers and participants were informed by explaining the purpose and methodology of the research, and their consents were obtained. It took about 5 minutes for each participant to complete the data collection tools. Data were evaluated by using SPSS 23.0 software in the computer environment. A p-value of < 0.05 was considered as statistically significant for this study. Chi-Square, Mann Whitney U, Kruskal Wallis, and Spearman Correlation Tests were used for data analysis.
Results
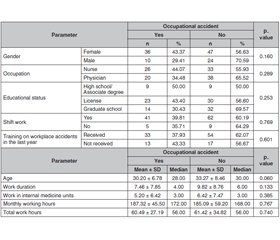
A total of 117 individuals, 83 women (70.94 %), and 34 men (29.06 %) participated in the study. Of the participants, 59 were nurses (50.43 %), and 58 were physicians (49.57 %). When the participants were examined according to their educational level, 53 (43.50 %) of the participants were a university, and 46 (39.32 %) were grad school graduates. Of the participants, 103 (88.03 %) were working with shifts, and 74.36 % were trained on occupational accidents in the last year. When the distribution of the workers according to their knowledge on the near-miss incidents was examined, 108 (92.31 %) knew what the near-miss incident is, and 95 of them (88.00 %) think that the near-miss incident reports are effective in reducing occupational accidents. Of the participants, 46 (39.32 %) experienced occupational accident. Of these events, 29 (63.04 %) happened in 08:00–16:00 shift, 13 (28.26 %) happened in 16:00–08:00 shift and 4 (8.70 %) happened in 08:00–08:00 shift. Of those who had a occupational accident, 34 (73.90 %) stated that they were wearing personal protective equipment when they were exposed to a occupational accident. Of the participants exposed to occupational accidents, 16 (34.78 %) reported the accident to the institution. When the participants were asked on the reasons for not reporting the accident to the institution, 15 participants (50.00 %) stated that they were very busy, 9 participants (30.00 %) considered that the accident was not risky for HIV-HBV-HCV infections, 8 participants (26.67 %) considered that it was not important to report, 5 participants (16.67 %) reported that the tool causing injury was not used in any patient and 3 participants (10.00 %) did not know that they should report the accident. Of those who had a occupational accident, 17 (36.96 %) reported that they exposed to occupational accident because of haste, fatigue (n = 17; 36.96 %), sleeplessness (n = 11; 23.91 %), patients movement (n = 8; 17.39 %), carelessness (n = 7; 15.22 %), and absent-mindedness (n = 6; 13.04 %). Of occupational accidents, 26 (56.52 %) were cutting-edge injuries, 20 (43.48 %) were exposed to violence, 13 (28.26 %) were exposed to blood and body fluids, 5 (10.87 %) were radiation exposure, and 3 (6.52 %) were fall-slip-injury (tables 1, 2).
/80.jpg)
/81.jpg)
Of 33 (28.21 %) participants who experienced the near-miss incident, 26 reported that they used personal protective equipment during the near-miss incident. Of the participants with near-miss event history, 19 (57.58 %) were in 08:00–16:00, 8 (24.24 %) were in 16:00–08:00 and 6 (18.18 %) were in 08:00–08:00 shifts. Of the 33 (12.50 %) participants experienced near-miss, only 4 reported the incident to the institution. When the participants were asked on the reasons for not reporting the incident, 12 (42.86 %) stated that they were very busy, 11 participants (39.29 %) did not know they should report the incident, 8 participants (28.57 %) stated that the tool they used during near-miss event was not used in any patient, 8 participants (28.57 %) thought that the patient was not risky regarding HIV-HBV-HCV infections, 6 participants (21.43 %) considered that it was not important to report, and 2 (7.14 %) could not report the near-miss incident due to lack of responsive unit for near-miss events within the hospital. The participants experienced near-miss events reported fatigue (n = 14; 43.75 %), haste (n = 13; 40.63 %), sleeplessness (n = 12; 37.50 %), absentmindedness(n = 7; 21.88 %), carelessness (n = 5; 15.63 %), medical device disruptions (n = 4; 12.50 %), patient movement (n = 4; 12.50 %), and lack of removal of contaminated instruments (n = 1; 3.13 %), as the causes of the events (tables 1, 2).
Of the near-miss events, 18 (54.55 %) were penetrating and piercing injuries, 14 (42.42 %) were exposed to blood and body fluids, 9 (27.27 %) were exposed to violence, 3 (9.09 %) were fall-sliding injury, 2 (6.06 %) were electrical medical device accident, and 2 (6.06 %) were radiation exposure. When occupational accident histories and characteristics of the participants were analyzed, it was observed that there was no significant relationship between occupational accident and participant characteristics (for all p > 0.05). There was no statistically significant relationship between having a occupational accident and the age and professional working duration of the participants (for all p > 0.05). It was observed that women had a higher incidence of near-miss events (33.73 %) compared to men (14.71 %) (p = 0.038). There was no statistically significant relationship between participant characteristics and near-miss events (p > 0.05). There was no statistically significant association between experiencing a near-miss event and the age and professional working duration of the participants (for all p > 0.05) (tables 3, 4).
/82.jpg)
/83.jpg)
There was a significant moderate positive correlation (r = 0.305) between age and the number of occupational accidents (p = 0.039). The number of occupational accidents increases with the increasing age of the participants. The average number of occupational accidents experienced by nurses (1.31 ± 0.74) was found to be lower than physicians (2.80 ± 2.53) (p = 0.006). It was also observed that there was a statistically significant relationship between educational status and the number of occupational accidents. The post hoc analysis showed that this significance was due to the difference between university and grad school graduates. The average number of occupational accidents of those with a postgraduate degree (3.36 ± 2.82) is higher than those with a university degree (1.26 ± 0.54) (p = 0.007). The average number of near-miss incidents experienced by men (6.60 ± 7.64) was found higher compared to women (1.36 ± 0.62) (p = 0.008). The number of near-miss incidents experienced by physicians (2.79 ± 4.30) was higher than the nurses (1.29 ± 0.83) (p = 0.032) (tables 5, 6).
/84.jpg)
Discussion
In this study, we aim to study the frequency of exposure to occupational accidents and near-miss events of the nurses and physicians working in the internal medicine units of a university hospital, and their reporting status and factors affecting these characteristics. We found in our study that increasing age of healthcare professionals in internal medicine units increase the occupational accidents. A previous study, Costa G. et al., showed that increasing age is associated with decreasing work ability index [15]. The shift work also wor-sens the health of aging personnel and may lead to sick shift worker effect [16]. Therefore, older personnel should be assigned to low-risk units for the prevention of occupational accidents.
According to our results, the number of occupational accidents and near-miss events experienced by physicians was higher than the nurses. In contrast, Pines et al. reported that physicians had the lowest frequency of occupational accidents, compared to workers in hospital housekeeping and maintenance departments. However, the severity of accidents experienced by physicians was higher compared to other workers [10]. Hence, we argue that specialized trai-ning in occupational accidents should be given to physicians. This intervention may include both physicians and nurses to increase their impact on both occupational accidents and near-miss events.
Our study demonstrated that women had a higher frequency to experience near-miss events; however, the number of near-miss events experienced by male participants were significantly higher. Further studies are required to conclude the effect of gender on near-miss events.
We found that the vast majority of healthcare professionals who experienced occupational accident did not use any protective equipment. According to a qualitative study executed by Neves et al. demonstrated, that the barriers against adherence to protective equipment are problems on communication, overwork, availability of protective equipment, and organizational issues [11]. Any educational intervention to prevent occupational accidents should include subjects focused on the use of protective equipment.
Our results showed that only a small fraction of participants reported their occupational accidents. This notification ratio falls to 12.50 % for reporting of near-miss events. Notification of occupational accidents and near-miss events are vital tools of epidemiology to analyze the health condition of workers, risk of occupational practices, and enable them to create strategies for health promotion. Secco et al. reported that guidance on healthcare professionals, according to the current legislation, is needed to enhance the notification flow [12]. Thus, we recommend that healthcare professionals should be informed on the importance of the notification of occupational accidents and near-miss events. Individual training and counseling should be provided to new physicians and nurses about reporting of occupational accidents and near-miss incidents.
Surprisingly, we found that most of the occupational accidents occur in the 08.00–16.00 shift. However, this result can be explained with a higher number of working personnel in day shifts. Previous studies showed that 8-hour shifts are safer compared to 10- or 12-hour shifts. Occupational injuries in afternoon shifts are relatively lower compared to morning shifts [21]. We recommend that the shifts should be organized as 8 hours shifts with appropriate rotations in shift periods. The shifts of aging or inexperienced personnel may be arranged as short afternoon shifts in order to minimalize the occupational accident risk.
Our results demonstrated that the most common causes of occupational accidents were fatigue/tiredness, haste, sleepiness, and absent-mindedness. A study executed on nurses working in private and university hospitals showed that the hospitals have problems in planning time schedules for nurses [22, 23]. Another study demonstrated that cognitive failures are linked to minor injuries and workplace accidents [15]. In addition to measures on ergonomic improvements, appropriate time schedules, and support on mindful nursing practices in a safe psychological environment may decrease workload and workplace accident frequency.
As our findings indicate, an important fraction of workplace accidents and near-miss events occur due to cuts and puncture wounds, which have a high risk of blood-borne infections. According to a previous study on healthcare professionals working in Nigeria, blood-related occupational accidents are associated with the inadequacy of protective measures and equipment, haste, and procedure types [16]. An adequate supply of protective equipment, ease of access to protective equipment, proper time management, and organization measures on prevention of cuts and puncture wounds may decrease the frequency of workplace accidents and near-miss incidents dramatically.
Conclusions
— As age increases, the number of occupational accidents also increases. Elderly personnel should be assigned to low-risk units in terms of preventing occupational accidents. The number of occupational accidents experienced by physicians and the number of near-misses were found to be higher than that of nurses. Physicians should be given special training on occupational accidents.
— Programs covering multi-faceted initiatives to prevent work accidents and near-misses should be organized and implemented in hospitals. Further research should be conducted to establish and demonstrate the effectiveness of programs aimed at preventing occupational accident risks of employees.
— The units that carry out the necessary work to notify the occupational accidents and near-misses and to take preventive measures should be introduced. Physicians and nurses should be included in training programs to report work accidents and near-misses to the relevant unit.
— Individual training and counseling should be provided to newly recruited physicians and nurses on occupational accidents and near-misses. Attention should be paid to the use of protective equipment. A healthy working environment should be created and adequate protective materials should be provided. Attention should be paid to each accident and it is necessary to question the accidents in detail and take precautions, considering that they give an idea about possible future accidents.
— Training of health professionals on health risks they may encounter and protective measures against occupational accidents have vital importance. However, further research should be carried out to create and improve training programs to prevent the risks of occupational accidents.
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Received 10.08.2021
Revised 27.08.2021
Accepted 15.09.2021

/80.jpg)
/81.jpg)
/82.jpg)
/83.jpg)
/84.jpg)