Международный эндокринологический журнал Том 18, №6, 2022
Вернуться к номеру
Яка причина високої смертності пацієнтів при RT-PCR-негативному COVID-19 на тлі супутніх захворювань?
Авторы: Mümtaz Taner Torun, Dilber Yilmaz Durmaz
Medical School, Bandirma Onyedi Eylul University, Bandirma, Balikesir, Turkey
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
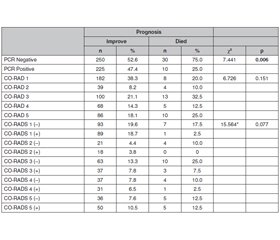
Актуальність. Пандемія COVID-19 вплинула на весь світ, однак досі не досягнуто достатнього прогресу в його діагностиці та лікуванні. Оскільки відсутній ефективний метод лікування COVID-19, рівень смертності надзвичайно високий, незважаючи на різні підходи до терапії. Рівень смертності від COVID-19 у Китаї становить 1,4–4,61 %, в Італії — 11,9 %, в Іспанії — 9,0 %, а у Великобританії — 7,9 %. Дослідження має на меті дослідити показники смертності серед пацієнтів із негативним RT-PCR COVID-19 на тлі супутніх захворювань. Матеріали та методи. У ретроспективне перехресне дослідження були включені пацієнти, які проходили лікування COVID-19 у клініці в період із березня 2020 року по березень 2021 року. Проведено аналіз медичної документації. Результати. Серед 515 пацієнтів діагностовані супутні захворювання: у 40,4 % — артеріальна гіпертензія (АГ), у 16,7 % — цукровий діабет, у 13 % — захворювання легень, у 28 % — ішемічна хвороба серця (ІХС), у 12,6 % — психічні захворювання, у 3,7 % — онкологічні захворювання та у 18,4 % — інші хвороби. Померли 40 пацієнтів (7,8 %), одужали — 475 (92,2 %). Більшість пацієнтів, які померли, мали негативний результат ПЛР-тесту (30 пацієнтів — 75 %), і ця різниця була значущою в статистичному аналізі на основі показника негативної полімеразної ланцюгової реакції з оберненою транскрипцією — RT-PCR (p = 0,006). Крім того, оцінюючи вплив супутніх захворювань на прогноз, виявили, що наявність АГ (p = 0,001), ІХС (p = 0,004) й астми та/або хронічного обструктивного захворювання легень (p = 0,019) була пов’язана з незадовільним прогнозом. Висновки. Установлено, що АГ, ІХС та хвороби легень пов’язані з поганим прогнозом при COVID-19. Крім того, слід підкреслити, що показники смертності в групі пацієнтів із негативним результатом RT-PCR були вищими. Пізнє звернення до клініки та затримка лікування можуть пояснити високі показники смертності в пацієнтів із негативною полімеразною ланцюговою реакцією з оберненою транскрипцією. Оцінка симптомів, дослідження комп’ютерної томографії грудної клітки та гематологічних даних, а також ранній початок лікування можуть знизити смертність у пацієнтів із негативним результатом RT-PCR.
Background. The COVID-19 pandemic has affected the whole world and still, sufficient progress has not been made in diagnosis and treatment. Since there has not been a definite method for the treatment of COVID-19 yet, the mortality rate is extremely high despite the different treatments. Mortality rates of COVID-19 in China are reported as 1.4–4.61%, in Italy — 11.9%, in Spain — 9.0%, and in the UK — 7.9%. The study purpose was to investigate the mortality rates in reverse transcriptase-polymerase chain reaction (RT-PCR) negative COVID-19 patients with comorbid the disease. Materials and methods. A retrospective cross-sectional study was conducted in the COVID-19 service. Patients who had COVID-19 treatment in our clinic between March 2020 and March 2021 were included in the study. A review of medical records was performed. Results. Comorbidity rates of the 515 patients were 40.4% hypertension (HT), 16.7% diabetes mellitus, 13% pulmonary diseases, 28% coronary artery disease (CAD), 12.6% psychiatric diseases, 3.7% oncological diseases and 18.4% other diseases. While 40 patients (7.8%) died, 475 patients (92.2%) recovered. Most of the patients who died were found to have a negative PCR test result (30 patients, 75%) and this difference was significant in the statistical analysis based on RT-PCR status (p = 0.006). Moreover, evaluating the effects of comorbid diseases on prognosis, it was found that HT (p = 0.001), CAD (p = 0.004), and asthma and/or chronic obstructive pulmonary disease (p = 0.019) were associated with poor prognosis. Conclusions. HT, CAD, and pulmonary diseases are supposed to be associated with poor prognosis. In addition, it is noteworthy that the mortality rates in the RT-PCR negative patient group were higher. Delay in clinic entry and delay in treatment may explain the high mortality rates in patients with negative RT-PCR. Evaluating the symptoms, examining chest CT and hematological data, and establishing treatment plans earlier can reduce mortality in RT-PCR negative patients.
пандемія COVID-19; смертність; цукровий діабет; супутні захворювання
COVID-19 pandemic; mortality rates; diabetes mellitus; comorbid diseases
Introduction
Materials and methods
Results
Discussion
Conclusions
- Kim H., Hong H., Yoon S.H. Diagnostic performance of CT and reverse transcriptase polymerase chain reaction for coronavirus disease 2019: A meta-analysis. Radiology. 2020. 296(3). 145-55. https://doi.org/10.1148/radiol.2020201343.
- Li Y., Yao L., Li J., Chen L., Song Y., Cai Z. et al. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J. Med. Virol. 2020. 92(7). 903-8. https://doi.org/10.1002/jmv.25786.
- Prokop M., vanEverdingen W., vanReesVellinga T., Quarles van Ufford H., Stöger L., Beenen L. et al. CO-RADS: A categorical CT assessment scheme for patients suspected of having COVID-19-Definition and evaluation. Radiology. 2020. 296(2). 97-104. https://doi.org/10.1148/radiol.2020201473.
- Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M. et al. COVID-19 and the cardiovascular system: Implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020. 116(10). 1666-87. https://doi.org/10.1093/cvr/cvaa106.
- Long D.R., Gombar S., Hogan C.A., Greninger A.L., OReilly Shah V., Bryson-Cahn C. et al. Occurrence and timing of subsequent SARS-CoV-2 RT-PCR positivity among initially negative patients. MedRxiv2020:2020.05.03.20089151. https://doi.org/doi: 10.1101/2020.05.03.20089151.
- Arevalo-Rodriguez I., Buitrago-Garcia D., Simancas-Racines D., Zambrano-Achig P., Del Campo R., Ciapponi A. et al. False-negative results of initial RT-PCR assays for COVID-19: A systematic review. PLoS One. 2020. 15(12). e0242958. https://doi.org/10.1371/journal.pone.0242958.
- Khatami F., Saatchi M., Zadeh S.S.T., Aghamir Z.S., Shabestari A.N., Reis L.O. et al. A meta-analysis of accuracy and sensitivity of chest CT and RT-PCR in COVID-19 diagnosis. Sci. Rep. 2020. 10(1). 22402. https://doi.org/10.1038/s41598-020-80061-2.
- Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P. et al. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020. 296(2). 115-7. https://doi.org/10.1148/radiol.2020200432.
- Fu Z., Tang N., Chen Y., Ma L., Wei Y., Lu Y. et al. CT features of COVID-19 patients with two consecutive negative RT-PCR tests after treatment. Sci. Rep. 2020. 10(1). 11548. https://doi.org/ 10.1038/s41598-020-68509-x.
- Chen H.J., Qiu J., Wu B., Huang T., Gao Y., Wang Z.P. et al. Early chest CT features of patients with 2019 novel coronavirus (COVID-19) pneumonia: relationship to diagnosis and prognosis. Eur. Radiol. 2020. 30(11). 6178-85. https://doi.org/10.1007/s00330-020-06978-4.
- Chen D., Jiang X., Hong Y., Wen Z., Wei S., Peng G. et al. Can Chest CT Features distinguish patients with negative from those with positive initial RT-PCR results for Coronavirus Disease (COVID-19)? Am. J. Roentgenol. 2021. 216(1). 66-70. https://doi.org/10.2214/AJR.20.23012.
- Tadic M., Cuspidi C., Grassi G., Mancia G. COVID-19 and arterial hypertension: Hypothesis or evidence? J. Clin Hypertens (Greenwich). 2020. 22(7). 1120-6. https://doi.org/10.1111/jch.13925.
- Meng M., Zhao Q., Kumar R., Bai C., Deng Y., Wan B. Impact of cardiovascular and metabolic diseases on the severity of COVID-19: A systematic review and meta-analysis. Aging (Albany NY). 2020. 12(22). 23409-234. https://doi.org/10.18632/aging.
- Kreutz R., Algharably E., Azizi M., Dobrowolski P., Guzik T., Januszewicz A. et al. Hypertension, the renin-angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for COVID-19. Cardiovasc. Res. 2020. 116(10). 1688-99. https://doi.org/10.1093/cvr/cvaa097.
- Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L. et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020. 109(5). 531-8. https://doi.org/ 10.1007/s00392-020-01626-9.
- Ceriello A. Hyperglycemia and the worse prognosis of COVID-19. Why a fast blood glucose control should be mandatory. Diabetes Res. Clin. Pract. 2020. 163. 108186. https://doi.org/10.1016/j.diabres.2020.108186.
- Buetti N., Trimboli P., Mazzuchelli T., Lo Priore E., Balmelli C., Trkola A. et al. Diabetes mellitus is a risk factor for prolonged SARS-CoV-2 viral shedding in lower respiratory tract samples of critically ill patients. Endocrine. 2020. 70(3). 454-60. https://doi.org/10.1007/s12020-020-02465-4.
- Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y. et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020. 146(1). 110-8. https://doi.org/10.1016/j.jaci.2020.04.006.
- Novel Coronavirus Pneumonia Emergency Response Epidemiology T. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020. 41(2). 145-51.
- Kuderer N.M., Choueiri T.K., Shah DP., Shyr Y., Rubinstein S.M., Rivera D.R. et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet. 2020. 395(10241). 1907-18. https://doi.org/10.1016/S0140-6736(20)31187-9.
- Yang K., Sheng Y., Huang C., Jin Y., Xiong N., Jiang K. et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020. 21(7). 904-13. https://doi.org/10.1016/S1470-2045(20)30310-7.
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. 323(11). 1061-9. https://doi.org/10.1001/jama.2020.1585.
- O’Driscoll M., Ribeiro Dos Santos G., Wang L., Cummings D.A.T., Azman A.S., Paireau J. et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021. 590(7844). 140-5. https://doi.org/10.1038/s41586-020-2918-0.
- Zhao Y., Zhao Z., Wang Y., Zhou Y., Ma Y., Zuo W. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv. 2020.01.26.919985. https://doi.org/ 10.1101/2020.01.26.919985.
- Baicry F., Le Borgne P., Fabacher T., Behr M., Lemaitre E.L., Gayol PA. et al. Patients with initial negative RT-PCR and typical imaging of COVID-19: Clinical implications. J. Clin. Med. 2020. 9(9). 3014. https://doi.org/10.3390/jcm9093014.
- Assaad S., Avrillon V., Fournier M.L, Mastroianni B., Russias B., Swalduz A. et al. High mortality rate in cancer patients with symptoms of COVID-19 with or without detectable SARS-COV-2 on RT-PCR. Eur. J. Cancer. 2020. 135. 251-9. https://doi.org/10.1016/ j.ejca.2020.05.028.
- Lascarrou J.B., Colin G., Le Thuaut A., Serck N., Ohana M., Sauneuf B. et al. Predictors of negative first SARS-CoV-2 RT-PCR despite final diagnosis of COVID-19 and association with outcome. Sci. Rep. 2021. 11(1). 2388. https://doi.org/10.1038/s41598-021-82192-6.

/21.jpg)
/22.jpg)